Published online Jun 28, 2010. doi: 10.3748/wjg.v16.i24.2971
Revised: March 3, 2010
Accepted: March 10, 2010
Published online: June 28, 2010
Systemic lupus erythematosus (SLE) is an autoimmune inflammatory disease characterized by the presence of a plethora of autoantibodies and immune complex formation. Virtually every system and organ can be affected by SLE. Gastrointestinal symptoms are common in SLE patients, and more than half of them are caused by adverse reactions to medications and viral or bacterial infections. Though not as common as lupus nephritis, SLE-related gastrointestinal involvement is clinically important because most cases can be life-threatening if not treated promptly. Lupus mesenteric vasculitis is the most common cause, followed by protein-losing enteropathy, intestinal pseudo-obstruction, acute pancreatitis and other rare complications such as celiac disease, inflammatory bowel diseases, etc. No specific autoantibody is identified as being associated with SLE-related gastroenteropathy. Imaging studies, particularly abdominal computed tomography scans, are helpful in diagnosing some SLE-related gastroenteropathies. Most of these complications have good therapeutic responses to corticosteroids and immunosuppressive agents. Supportive measures such as bowel rest, nutritional support, antibiotics and prokinetic medications are helpful in facilitating functional recovery and improving the outcome.
- Citation: Tian XP, Zhang X. Gastrointestinal involvement in systemic lupus erythematosus: Insight into pathogenesis, diagnosis and treatment. World J Gastroenterol 2010; 16(24): 2971-2977
- URL: https://www.wjgnet.com/1007-9327/full/v16/i24/2971.htm
- DOI: https://dx.doi.org/10.3748/wjg.v16.i24.2971
Systemic lupus erythematosus (SLE) is a systemic autoimmune inflammatory disease with protean clinical manifestations. The gastrointestinal tract is one of the most commonly affected systems in SLE. However, most gastrointestinal manifestations are caused by adverse reactions from therapeutic agents and infections, while the symptoms related to the disease per se are not as common as other organ involvement such as lupus nephritis[1-6]. On the other hand, the incidence of gastrointestinal manifestations may be underestimated clinically because some of them are indistinct and may not have abdominal symptoms. One autopsy study found that 60%-70% of SLE patients had evidence of peritonitis, whereas only around 10% of them were recognized clinically[1]. It is noteworthy that gastrointestinal vasculitis and thrombosis can lead to life-threatening ischemia, perforation and infarction, and surgical interventions are usually needed if not treated promptly with immunosuppressant. In this paper, clinically important gastrointestinal complications of SLE are reviewed for the purpose of improving treatment efficacy and outcome.
A number of terms have been used to describe lupus mesenteric vasculitis (LMV), including mesenteric arteritis, lupus enteritis, lupus arteritis, lupus vasculitis, gastrointestinal vasculitis, intra-abdominal vasculitis and acute gastrointestinal syndrome. LMV is one of the main causes of acute abdominal pain in SLE patients. It can be classified into an acute ischemic enteritis that involves mainly small intestine and chronic multiple ulcers occurring mainly in the colon[2]. About 8%-40% of SLE patients have acute abdominal pain during the stage of active disease[3], but LMV is generally an uncommon condition in SLE patients. In Asia, the reported overall prevalence of LMV in patients with SLE is 2.2%-9.7%[4-6]. However, the prevalence of LMV in America seems to be much lower: 0.9%[7]. Ju et al[8] reported that the global prevalence of LMV ranges from 0.2% to 9.7% among all SLE patients and from 29% to 65% in patients who had acute abdominal pain. LMV occurs almost always in patients with active disease[6].
The predisposing factors for LMV are unknown. The proposed trigger factors include bacterial infections that lead to changes of intestinal flora, cytomegalovirus infection, eosinophilia, non steroidal anti-inflammatory drugs, chemicals, metallic particulates, animal viruses, helminth infection, caffeine, phosphodiesterase-4-inhibitors, adenosine diphosphate, certain foods and herbal medicines[6].
Inflammatory vasculitis secondary to immune complex deposition and thrombosis of the intestinal vessels secondary to circulating anti-phospholipid antibodies are the proposed pathogenic mechanisms of LMV[9-12]. Both types of microvasculopathy can activate each other reciprocally, resulting in worsening cascades of vasculitis and thrombosis. Autoantibodies, such as lupus anticoagulant, anti-cardiolipin antibody and anti-β2-glycoprotein antibody, are associated with LMV. A study suggests that some cryptic antigens which can stimulate the production of anti-endothelial antibodies are exposed when endothelial cells are disrupted[10]. In a study by Kwok et al[6], the authors found that the serum levels of anti-endothelial cell IgG were significantly higher in SLE patients with LMV than in those without LMV or in healthy controls. Macroscopically, the appearance of LMV varies from segmental edema to ulceration, gangrene and perforation[8]. Both small arteritis and venulitis are found in LMV. Microscopically, fibrinoid necrosis of subserosal vessels and leukocytoclasis on the vascular wall, as well as edematous submucosa with mild diffuse inflammatory infiltration of mononuclear cells, can be observed. In the muscular layer, intravascular fibrin thrombus and hemorrhage around the small veins can be found.
Both the inflammatory and thrombotic mesenteric vasculopathy of LMV can cause mesenteric ischemia. LMV can cause very severe abdominal symptoms and signs and sometimes is diagnosed as acute surgical abdomen. Typically, the abdominal pain caused by LMV is diffuse in pattern, in some cases accompanied by rebound tenderness and abdominal muscle guarding. The symptoms of LMV vary from mild, nonspecific abdominal pain, bloating or loose stool, to necrosis and intestinal perforation which manifest as severe extensive gastrointestinal bleeding or acute surgical abdomen. It is noteworthy that in LMV patients with bowel perforation, the typical signs can be absent. Other manifestations of LMV include anorexia, nausea, vomiting, dysphagia, hematemesis, postprandial fullness, diarrhea and melena. Kishimoto et al[13] reported two cases of “acute gastrointestinal distress syndrome”. Patients with this syndrome have recurrent lupus enteritis on the basis of mesenteric vasculopathy characterized by reversible intestinal wall edema accompanied by significant hypocomplementemia. These attacks are not complicated by bowel infarction, perforation or hematachezia and respond quickly to corticosteroid treatment.
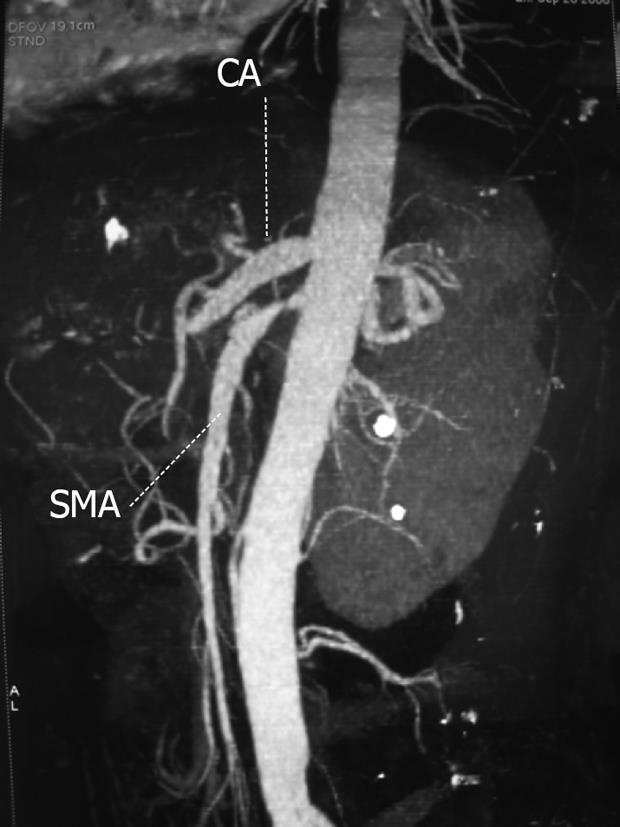
Accurate diagnosis of LMV is critical to allow prompt treatment to avoid unnecessary surgical intervention. As the clinical symptoms and laboratory parameters are non-specific, and bowel specimens are not always available, the diagnosis of LMV relies on abdominal computed tomography (CT) scan which allows both the bowel wall and the abdominal vasculature to be visualized. Advances in CT technology have been extremely helpful in detecting ischemia and for evaluating the causes of abdominal pain.
Common CT findings in patients with LMV include dilated bowel, focal or diffuse bowel wall thickening, abnormal bowel wall enhancement which is also called “target sign”, mesenteric edema, stenosis or engorgement of mesenteric vessels which is also called “the comb sign” and ascites (Figure 1). Segmental or multifocal involvement of the small and large bowel loops with intervening normal bowel segments indicates ischemic change, which is almost always indicative of vasculitis.
Ultrasonography is also useful for both the diagnosis and follow-up of LMV. Small intestinal wall edema and thickening can be visualized under ultrasonography. Irregular thickening and projection of folds in multiple segments of the duodenum and the terminal ileum accompanied by “thumb print” signs in double-contrast radiography suggest ischemic changes. Gastroscopy and colonoscopy can show ischemia and ulcerative changes. However, endoscopy-guided biopsy might not yield a definitive diagnosis of LMV because the affected vessels are usually located in an inaccessible area. Laparoscopy can be used in the diagnosis of LMV[8,9].
Early diagnosis and appropriate intervention can avoid potentially fatal complications of LMV. Because the primary lesions of LMV are inflammatory ischemic vasculitis, immediate and aggressive anti-inflammatory immunosuppressive treatment should be initiated as soon as the diagnosis of LMV is made. The treatments include high dose intravenous infusion of methylprednisolone or an equivalent agent and complete bowel rest. For patients with recurrent LMV and those who do not have adequate response to intravenous prednisolone alone, intravenous cyclophosphamide should be initiated. The initial dosage of cyclophosphamide is 1 mg/kg daily and the dosage is gradually tapered when LMV is stabilized[6]. In Kim’s study, they found that a bowel wall thickness greater than 9 mm usually indicated the presence of recurrent LMV and should be considered a high risk factor for recurrence[14]. They suggested that for patients with high risk of recurrence, immunosuppressive agents should be initiated as early as possible.
When a rapid response to immunosuppressive therapy is not achieved, surgical intervention for possible bowel perforation or large area of ischemia should be considered. Early laparotomy within 24 to 48 h is critical for improving the prognosis of LMV patients. Medina et al[15] found that 10 of 11 LMV patients who underwent surgery after 48 h died, while none of 33 patients who were operated on within 24-48 h died.
The prognosis of LMV varies in reports from different areas of the world. This might be due to genetic differences. Reports from Europe and North America indicate that the prognosis of LMV is poor and some fatalities can occur. Some reports claimed that the mortality of LMV could be as high as 50%[6,15]. The prognosis of LMV depends on the extent of vascular involvement, the prompt implementation of immunosuppressive therapy, and the time of surgical intervention. On the basis of published reports, the prognosis of LMV can be improved if abdominal CT is used to aid the diagnosis and if prompt immunosuppressive therapy is implemented.
Protein-losing gastroenteropathy (PLGE) is a condition characterized by profound edema and severe hypoalbuminemia secondary to excessive loss of serum protein from the gastrointestinal tract, clinically indistinguishable from nephrotic syndrome. Clinically significant PLGE seems uncommon in SLE. Besides two large series reported by Mok and our group with 16 and 15 patients respectively, most are isolated case reports or small series[16,17]. So far, less than 60 patients with SLE-related PLGE have been reported in the literature, and the majority of these patients are Asians; whether this is due to genetics or environmental factors remains to be elucidated. In Mok’s study, the point prevalence of their Chinese patients is 3.2% for PLGE, while in our series the prevalence is 1.9%. PLGE may occur in SLE patients of any age and occurs with a female predominance. In most circumstances, the typical features of PLGE develop before the diagnosis of SLE. In our study, 53.3% of patients had PLGE as the initial presentation of SLE, but PLGE could also occur 17 years after the establishment of SLE[17]. Gornisiewicz et al[18] have concluded that PLGE often happens in patients with clinically severe SLE with multiple system involvement.
The exact pathogenesis of SLE-related PLGE is still unclear. Mucosal ulceration, non-necrotizing mesenteric or intestinal blood vessel vasculitis, increase in capillary permeability caused by intravascular activation and conversion of complement, cytokine- (such as tumor necrosis factor-α and interleukin-6) or complement-mediated vascular or mucosal damage, and intestinal lymphangiectasia have been postulated as the pathogenic mechanisms[16,19].
The most predominant clinical manifestation of PLGE is profound peripheral pitting edema. Patients may have pleural, pericardial effusion and ascites due to severe hypoalbuminemia. Nausea, vomiting and diarrhea are also common in these patients. Diarrhea is present in 50% of cases, which is generally liquid in nature and can be as frequent as 20 times a day, but steatorrhea is absent[17,20]. No particular autoantibodies have been found to be associated with PLGE. Severe hypoalbuminemia and hypocomplementemia are the most predominant laboratory findings of PLGE. Kim et al[19] found in their study that hypercholesterolemia was common in SLE-related PLGE, but rare in idiopathic PLGE[16]. This might be due to the leakage of cholesterol-rich lipoprotein particles in the intestinal lymph. Most PLGE patients also have hypoglobulinemia because immunoglobulin can also leak into the intestinal lumen. The presence of anti-dsDNA and anti-ENA antibodies is not significantly different from patients without PLGE. Eighty percent of PLGE in our series occurred at the stage of active lupus, and non-specific chronic inflammation were detected in all pathological specimens obtained.
The diagnosis of SLE-related PLGE mainly relies on the exclusion of other causes of hypoalbuminemia such as lupus nephritis, abnormal liver function, decreased protein synthesis or malabsorption. In recent years, Tc-99m albumin scintigraphy has become the most frequently used diagnostic method. It is noninvasive and safe in demonstrating gastrointestinal loss of blood albumin to intestinal lumen. It also has the potential to localize protein leakage and can be used to monitor the efficacy of treatment. Gastroenteroscopy is usually not diagnostic, as 50% of SLE-related PLGE patients present with non-specific intestinal wall edema and 10% of patients have no abnormalities under endoscopy examination[21]. Histologically, lymphangiectesia, edematous villi and non-specific inflammation can be found in the intestine, but histology can also be normal because of the inaccessibility of the involved area under gastroendoscopy. An elevated α-1 antitrypsin can be used as a diagnostic alternative[22].
Due to limited number of patients, there is no controlled clinical trial to demonstrate the efficacy of treatment for SLE-related PLGE. Corticosteroid is the mainstay of treatment. Response to corticosteroid alone is excellent in more than 60% of patients. For those refractory to steroid, immunosuppressive agents such as azathioprine, cyclosporine A and cyclophosphamide could be added into the therapeutic regimen. Albumin infusion, nutritional support and diuretics are used as supplemental measures for the treatment. Octreotide can reduce intestinal microvasculature blood flow, decrease local lymph formation and ameliorate lymphatic dilatation, therefore can also be used in the treatment of PLGE. In addition, octreotide has immunomodulatory effects since it specifically binds with the somatostatin receptor. Prophylaxis for thromboembolic complications with warfarin should be considered in patients with severe and persistent protein loss, especially if antiphospholipid antibodies are present[16-18,20].
The outcome of most SLE-related PLGE cases is generally good since most patients respond well to steroid therapy. Relapse of PLGE occurs in 20%-30% of patients, particularly in patients undergoing maintenance therapy with low-dose prednisolone alone, but they respond again to an increased dosage of steroid. Mok et al[16] suggested that long-term maintenance treatment with low dose prednisolone plus azathioprine could reduce the rate of recurrence.
SLE-related intestinal pseudo-obstruction (IPO) is a rare but well-recognized clinical syndrome that reflects the dysfunction of the visceral smooth muscle, the enteric nerve and/or the visceral automatic nervous system[23]. It usually coincides with ureterohydronephrosis and/or interstitial cystitis, rarely with biliary dilatation (megacholedochus)[24]. IPO is associated with ureterohydronephrosis in 63.3% of cases[25]. IPO may appear during the course of SLE, but it can also be the initial presentation of SLE[26]. It usually occurs in patients with active lupus. So far, only 28 cases have been reported in the English literature; half of the cases were Oriental and female patients predominated[23].
The pathogenesis of SLE-related IPO is unknown. Histopathological evidence of intestinal leiomyocyte damage suggests a systemic autoimmune process targeting smooth muscle cells[24]. Vasculitis leading to chronic ischemia of the bowel smooth muscle, which in turn leads to muscular damage and hypomotility, has been postulated as one of the possible mechanisms. Another possible mechanism is an intrinsic muscle dysmotility affecting the muscularis propria. The apparently high association between pseudo-obstruction and ureterohydronephrosis suggests a possible common smooth muscle dysmotility due to primary myopathy or neurogenic pathology, secondary to either immune complex-mediated vasculitis or common circulating autoantibodies against smooth muscle. Biopsied specimens have shown fibrotic process and atrophy in the muscularis layer, decreased number of smooth muscle cells and inflammatory cell infiltration associated with fibrinoid deposits, indicative of vasculitis[26].
The characteristic clinical manifestation of IPO is ineffective intestinal propulsion with the presence of clinical features of intestinal obstruction without an identifiable organic obstructive lesion and an abdominal distension with a very sluggish or absent peristalsis. Antroduodenal manometry demonstrates intestinal hypomotility and esophageal aperistalsis. Symptoms of IPO include a subacute onset of abdominal pain, nausea and vomiting, abdominal distension, constipation, diarrhea and weight loss. Laboratory findings are non-specific. Anti-proliferative cell nuclear antigen antibody (anti-PCNA) was found to be more frequently detected than in lupus patients without IPO in one study[27]. Mok et al[28] reported that SLE-related IPO patients had higher frequency of positive anti-Ro and anti-RNP antibodies compared to lupus patients without IPO.
Radiological examination can detect dilated fluid-filled bowel loops, with thickened bowel wall and multiple fluid levels. Bilateral ureter dilatation with a reduced urinary bladder capacity can be found if ureterhydronephrosis is the concurrent situation. Abdominal CT scan frequently reveals the presence of dilated small and large bowel with thickened intestinal wall.
Pathological examination of the gastrointestinal tract of SLE-related IPO patients can reveal widespread myocyte necrosis in the muscularis propria with active inflammatory cell infiltration, severe atrophy of muscularis, active serositis with serosal thickening and fibrosis, but little or no evidence of vasculitis and absence of thromboembolism.
The diagnosis of this clinical syndrome is based on imaging findings consistent with the presence of dilated small and large bowel loops with thickened intestinal wall and multiple fluid levels. Other possible causes of intestinal obstruction should be excluded. Invasive diagnostic procedures should be avoided.
Corticosteroids, immunosuppressive agents combined with supportive measures such as parenteral nutrition, oral broad-spectrum antibiotics to diminish bacteria overgrowth and pharmacological stimulation of small bowel motility are effective medical management options for SLE-related IPO. Timely diagnosis and early intervention are critical to rehabilitate the peristaltic activity of both the gastrointestinal tract and the genitourinary viscera; delayed treatment has been associated with failure to regain functional peristalsis and leads to histopathological progression to fibrosis and atrophy of the intestinal wall, and secondary impairment of the myenteric plexuses[24]. SLE-related IPO usually responds well to high dose corticosteroids. Erythromycin in particular is the appropriate antibiotic in this situation due to its prokinetic effect. Other prokinetic agents such as cisapride and octreotide are also helpful in stimulating small bowel motility. Octreotide appears to be effective in improving both clinical symptoms and manometric patterns[26]. Azathioprine, cyclophosphamide and cyclosporine A are the immunosuppressive agents that could be used as one component of a maintenance therapeutic regimen with oral corticosteroids. Other immunosuppressive agents against B cells, immune complex formation and pathogenic autoantibody formation could be the alternatives.
High dose intravenous corticosteroid treatment is effective in most patients, leading to clinical remission and disappearance of abnormal imaging findings. Long-term outcome of SLE-related IPO varies. Some patients may have recurrent attacks of IPO without other major organ involvement despite maintenance treatment with steroids and immunosuppressive agents. The reported mortality rate is 18%[26]. Early diagnosis and prompt treatment is critical to improve the overall outcome of SLE-related IPO patients.
About 160 cases of SLE-related acute pancreatitis have been reported in the literature. Pancreatitis is a rare but life-threatening complication of SLE and our knowledge about this complication is mainly based on individual case reports. Based on the literature reports, the annual incidence of SLE-related pancreatitis is estimated to be 0.4-1.1/1000 lupus patients[29,30]. Reports from Europe and the United States showed that the rate of pancreatitis with SLE is between 0.7%-4%[31,32]. However, the rate of SLE-related pancreatitis may be underestimated because cases of subclinical pancreatitis with elevated pancreatic enzymes but no symptoms are not diagnosed or reported. It is estimated that 30.5% of asymptomatic SLE patients have hyperamylasemia[33].
Sixty percent of cases develop acute pancreatitis within 2 years of the diagnosis of lupus, and in 22% of patients, pancreatitis is the initial clinical presentation. In most cases, acute pancreatitis is associated with active lupus. In addition to traditional predisposing factors such as hypertriglyceridemia, steroid and azathioprine use were proposed as the possible causes of pancreatitis in lupus patients. However, in Pascual-Ramos’s study, they could not prove the association between steroid and/or azathioprine administration and the development of pancreatitis even after they “rechallenged” the onset of pancreatitis with these medications[34].
The pathogenic mechanism of SLE-related pancreatitis is unclear. Vascular damage has been stressed as a cause of this problem. Necrotizing vasculitis, occlusion of arteries and arterioles by thrombi resulting from severe hypertension or antiphospholipid syndrome, intimal thickening and proliferation and immune complex deposition with complement activation in the wall of pancreatic arteries have been postulated[31]. Sixteen specimens of pancreatic tissue from SLE-related pancreatitis patients were examined in one series; evidence of inflammation and necrosis could be found in all specimens, but vasculitis could only be found in one case[31]. It is possible that an autoimmune reaction involving abnormal cellular immune response or antibody reaction, rather than vasculitis, is responsible for the inflammation reaction.
Eighty-eight percent of SLE-related pancreatitis cases have abdominal pain; in only 23% of them the pain radiates to the back. Two-thirds of patients have nausea and vomiting, and half of them have fever. Diarrhea is uncommon and a few patients have panniculitis.
Elevated serum amylase and lipase are the most commonly detected biochemical abnormalities. Additional biochemical abnormalities include hypoalbuminemia, abnormal liver function tests, elevated serum creatinine and hypocalcemia. Anti-La antibody is the only autoantibody reported to be associated with this particular complication[32].
The diagnosis is based on the laboratory evidence of elevated serum amylase or lipase levels. Clinical symptoms and suggestive tomographic findings are helpful. However, lupus patients may develop acute pancreatitis secondary to other “non-SLE” causes such as mechanical (including cholelithiasis), toxic chemicals (such as alcohol ingestion, some medications), hypertriglycemia and hypocalcemia, as well as viral infections or sepsis. The diagnosis of SLE-related pancreatitis can only be confirmed when these possible causes are excluded.
Corticosteroids should be used as the medical management of SLE-related acute pancreatitis as long as this drug can be excluded as the cause of pancreatitis. Immunosuppressive agents such as azathioprine or cyclophosphamide can be used in combination with corticosteroid. In severe cases, plasmapheresis and intravenous gamma-globulin infusion may be helpful.
As many as 57% of SLE-related acute pancreatitis cases may develop complications if not treated promptly[30]. Many of these complications can be fatal, with a mortality rate of 45%, whereas it is only 3% in patients without complications. Lupus activity is significantly associated with increased mortality. It is reported that SLE-related acute pancreatitis concurrent with central nervous system and cardiac involvement has the highest mortality rate. Increased serum creatinine, hypoalbuminemia, anti-DNA antibodies, thrombocytopenia, low complement, hypocalcemia, hyperglycemia and elevated liver enzymes are risk factors for increased mortality.
About 22% of patients may experience recurrent acute pancreatitis attacks, while 12% of patients develop pancreatic pseudocysts and 5%-14% become chronic[30,32].
The coexistence of SLE and celiac disease is rare. So far, only 17 cases have been reported in the literature. Both diseases have an autoimmune nature and share HLA-B8 and HLA-DR3 histocompatibility antigens[35]. Celiac disease can occur before or after the diagnosis of lupus[36]. Most patients have positive serum antigliadin antibodies and histological findings of duodenal biopsy which are consonant with celiac disease. Patient’s response to steroid along with gluten-free diet is excellent. The prognosis is generally good.
The coexistence of SLE and inflammatory bowel disease (IBD) is difficult to diagnose since both diseases share some common gastrointestinal features and some medications used in treating IBD may cause drug-induced lupus. The estimated prevalence of ulcerative colitis (UC) in SLE patients is around 0.4%[37]. So far, 27 cases of SLE-related UC have been reported, and numbers of SLE-related Crohn’s disease are even less. UC may occur either before or after the diagnosis of SLE. The majority of patients have excellent response to steroids combined with hydroxychloroquine or azathioprine. However, some patients with Crohn’s disease may have life-threatening massive gastrointestinal bleeding and need high dosage methylprednisolone[38]. The prognosis of SLE-related IBD is usually good.
Eosinophilic enteritis is a rare clinical condition. SLE-related eosinophilic enteritis is even rarer. Only 3 cases of SLE-related eosinophilic enteritis have been reported in the literature[39]. The clinical symptoms include abdominal pain, nausea, vomiting and sometimes diarrhea. Peripheral hypereosinophilia presents in most of the patients. The diagnosis depends on clinical symptoms and intestinal biopsy which shows eosinophils in the deep layers of the intestinal wall[39]. The recommended treatment regimen is prednisone 0.5-1 mg/kg per day in divided doses for 7-10 d followed by slow tapering over 2 to 3 mo. Immunosuppressive agents can be used in patients with recurrence or corticosteroid non-responders.
This is an uncommon disorder characterized by the presence of gas within the walls of the gastrointestinal tract. The most common rheumatic disease that is associated with pneumatosis cystoides intestinalis (PCI) is systemic sclerosis. Only 14 SLE-related PCI cases have been reported in the literature. It might be caused by injury of the mucosa and immune barrier due to lupus vasculitis and impaired healing due to corticosteroid therapy[40]. Pathological evidence of vasculitis can be found in at least half of the patients. Increased intraluminal pressure, mucosal injury and production of gas from bacteria in the mucosa may be involved in the pathogenesis of SLE-related PCI. The diagnosis depends on the abdomen findings on CT, which show thickened bowel walls with multiple linear and cystic radiolucencies. Therapeutic strategy for each PCI patient should be individualized. Oxygen inhalation or hyperbaric oxygen therapy is reported to promote removal of the gas from the cysts. Antibiotics are effective in reducing bacterial overgrowth and gas production. Bowel rest and prokinetic agents are the supportive measures in treating patients with SLE-related PCI.
Gastrointestinal manifestations are common in SLE patients, but most of them are due to adverse reactions to medications and infection. SLE-related gastrointestinal involvement is not rare, and sometimes can be life-threatening. Most SLE-related gastrointestinal complications are caused by vasculitis and immune complex deposition, and respond well to corticosteroids and immunosuppressive agents. Early diagnosis and timely treatment are critical to improve the prognosis. Supportive measures such as bowel rest are beneficial, and in some situations such as IPO and PCI antibiotics are helpful to facilitate functional restoration.
Peer reviewers: Dr. José Liberato Ferreira Caboclo, Professor, Rua Antônio de Godoy, 4120, São José do Rio Preto, Brazil; Teng-Yu Lee, MD, Division of Gastroenterology and Hepatology, Department of Internal Medicine, Taichung Veterans General Hospital, 160, Sec. 3, Taichung Harbor Road, Taichung 407, Taiwan, China; Weekitt Kittisupamongkol, MD, Hua Chiew Hospital, 665 Bumrungmuang Road, Bangkok 10100, Thailand
S- Editor Tian L L- Editor Logan S E- Editor Lin YP
| 1. | Takeno M, Ishigatsubo Y. Intestinal manifestations in systemic lupus erythematosus. Intern Med. 2006;45:41-42. [Cited in This Article: ] |
| 2. | Endo H, Kondo Y, Kawagoe K, Ohya TR, Yanagawa T, Asayama M, Hisatomi K, Teratani T, Yoneda M, Inamori M. Lupus enteritis detected by capsule endoscopy. Intern Med. 2007;46:1621-1622. [Cited in This Article: ] |
| 3. | Prouse PJ, Thompson EM, Gumpel JM. Systemic lupus erythematosus and abdominal pain. Br J Rheumatol. 1983;22:172-175. [Cited in This Article: ] |
| 4. | Lee CK, Ahn MS, Lee EY, Shin JH, Cho YS, Ha HK, Yoo B, Moon HB. Acute abdominal pain in systemic lupus erythematosus: focus on lupus enteritis (gastrointestinal vasculitis). Ann Rheum Dis. 2002;61:547-550. [Cited in This Article: ] |
| 5. | Lian TY, Edwards CJ, Chan SP, Chng HH. Reversible acute gastrointestinal syndrome associated with active systemic lupus erythematosus in patients admitted to hospital. Lupus. 2003;12:612-616. [Cited in This Article: ] |
| 6. | Kwok SK, Seo SH, Ju JH, Park KS, Yoon CH, Kim WU, Min JK, Park SH, Cho CS, Kim HY. Lupus enteritis: clinical characteristics, risk factor for relapse and association with anti-endothelial cell antibody. Lupus. 2007;16:803-809. [Cited in This Article: ] |
| 7. | Buck AC, Serebro LH, Quinet RJ. Subacute abdominal pain requiring hospitalization in a systemic lupus erythematosus patient: a retrospective analysis and review of the literature. Lupus. 2001;10:491-495. [Cited in This Article: ] |
| 8. | Ju JH, Min JK, Jung CK, Oh SN, Kwok SK, Kang KY, Park KS, Ko HJ, Yoon CH, Park SH. Lupus mesenteric vasculitis can cause acute abdominal pain in patients with SLE. Nat Rev Rheumatol. 2009;5:273-281. [Cited in This Article: ] |
| 9. | Helliwell TR, Flook D, Whitworth J, Day DW. Arteritis and venulitis in systemic lupus erythematosus resulting in massive lower intestinal haemorrhage. Histopathology. 1985;9:1103-1113. [Cited in This Article: ] |
| 10. | Del Papa N, Guidali L, Sala A, Buccellati C, Khamashta MA, Ichikawa K, Koike T, Balestrieri G, Tincani A, Hughes GR. Endothelial cells as target for antiphospholipid antibodies. Human polyclonal and monoclonal anti-beta 2-glycoprotein I antibodies react in vitro with endothelial cells through adherent beta 2-glycoprotein I and induce endothelial activation. Arthritis Rheum. 1997;40:551-561. [Cited in This Article: ] |
| 11. | Simantov R, LaSala JM, Lo SK, Gharavi AE, Sammaritano LR, Salmon JE, Silverstein RL. Activation of cultured vascular endothelial cells by antiphospholipid antibodies. J Clin Invest. 1995;96:2211-2219. [Cited in This Article: ] |
| 12. | Cervera R, Espinosa G, Cordero A, Oltra MR, Unzurrunzaga A, Rossiñol T, Plaza J, Bucciarelli S, Ramos-Casals M, Ingelmo M. Intestinal involvement secondary to the antiphospholipid syndrome (APS): clinical and immunologic characteristics of 97 patients: comparison of classic and catastrophic APS. Semin Arthritis Rheum. 2007;36:287-296. [Cited in This Article: ] |
| 13. | Kishimoto M, Nasir A, Mor A, Belmont HM. Acute gastrointestinal distress syndrome in patients with systemic lupus erythematosus. Lupus. 2007;16:137-141. [Cited in This Article: ] |
| 14. | Kim YG, Ha HK, Nah SS, Lee CK, Moon HB, Yoo B. Acute abdominal pain in systemic lupus erythematosus: factors contributing to recurrence of lupus enteritis. Ann Rheum Dis. 2006;65:1537-1538. [Cited in This Article: ] |
| 15. | Medina F, Ayala A, Jara LJ, Becerra M, Miranda JM, Fraga A. Acute abdomen in systemic lupus erythematosus: the importance of early laparotomy. Am J Med. 1997;103:100-105. [Cited in This Article: ] |
| 16. | Mok CC, Ying KY, Mak A, To CH, Szeto ML. Outcome of protein-losing gastroenteropathy in systemic lupus erythematosus treated with prednisolone and azathioprine. Rheumatology (Oxford). 2006;45:425-429. [Cited in This Article: ] |
| 17. | Zheng WJ, Tian XP, Li L, Jing HL, Li F, Zeng XF, Tang FL. Protein-losing enteropathy in systemic lupus erythematosus: analysis of the clinical features of fifteen patients. J Clin Rheumatol. 2007;13:313-316. [Cited in This Article: ] |
| 18. | Gornisiewicz M, Rodriguez M, Smith JK, Saag K, Alarcón GS. Protein-losing enteropathy in a young African-American woman with abdominal pain, diarrhea and hydronephrosis. Lupus. 2001;10:835-840. [Cited in This Article: ] |
| 19. | Kim YG, Lee CK, Byeon JS, Myung SJ, Oh JS, Nah SS, Moon HB, Yoo B. Serum cholesterol in idiopathic and lupus-related protein-losing enteropathy. Lupus. 2008;17:575-579. [Cited in This Article: ] |
| 20. | Hung J, Wood CA, Woronik V, Vieira JM Jr, Barros RT. Protein-losing gastroenteropathy in a patient with systemic lupus erythematosus and antiphospholipid antibody syndrome simulating nephrotic syndrome. Nephrol Dial Transplant. 2006;21:2027-2028. [Cited in This Article: ] |
| 21. | Yazici Y, Erkan D, Levine DM, Parker TS, Lockshin MD. Protein-losing enteropathy in systemic lupus erythematosus: report of a severe, persistent case and review of pathophysiology. Lupus. 2002;11:119-123. [Cited in This Article: ] |
| 22. | Oh DC, Ng TM, Ho J, Leong KP. Systemic lupus erythematosus with concurrent protein-losing enteropathy and primary sclerosing cholangitis: a unique association. Lupus. 2006;15:102-104. [Cited in This Article: ] |
| 23. | Pardos-Gea J, Ordi-Ros J, Selva A, Perez-Lopez J, Balada E, Vilardell M. Chronic intestinal pseudo-obstruction associated with biliary tract dilatation in a patient with systemic lupus erythematosus. Lupus. 2005;14:328-330. [Cited in This Article: ] |
| 24. | Park FD, Lee JK, Madduri GD, Ghosh P. Generalized megaviscera of lupus: refractory intestinal pseudo-obstruction, ureterohydronephrosis and megacholedochus. World J Gastroenterol. 2009;15:3555-3559. [Cited in This Article: ] |
| 25. | Alexopoulou A, Andrianakos A, Dourakis SP. Intestinal pseudo-obstruction and ureterohydronephrosis as the presenting manifestations of relapse in a lupus patient. Lupus. 2004;13:954-956. [Cited in This Article: ] |
| 26. | Ceccato F, Salas A, Góngora V, Ruta S, Roverano S, Marcos JC, Garcìa M, Paira S. Chronic intestinal pseudo-obstruction in patients with systemic lupus erythematosus: report of four cases. Clin Rheumatol. 2008;27:399-402. [Cited in This Article: ] |
| 27. | Nojima Y, Mimura T, Hamasaki K, Furuya H, Tanaka G, Nakajima A, Matsuhashi N, Yazaki Y. Chronic intestinal pseudoobstruction associated with autoantibodies against proliferating cell nuclear antigen. Arthritis Rheum. 1996;39:877-879. [Cited in This Article: ] |
| 28. | Mok MY, Wong RW, Lau CS. Intestinal pseudo-obstruction in systemic lupus erythematosus: an uncommon but important clinical manifestation. Lupus. 2000;9:11-18. [Cited in This Article: ] |
| 29. | Breuer GS, Baer A, Dahan D, Nesher G. Lupus-associated pancreatitis. Autoimmun Rev. 2006;5:314-318. [Cited in This Article: ] |
| 30. | Nesher G, Breuer GS, Temprano K, Moore TL, Dahan D, Baer A, Alberton J, Izbicki G, Hersch M. Lupus-associated pancreatitis. Semin Arthritis Rheum. 2006;35:260-267. [Cited in This Article: ] |
| 31. | Lariño Noia J, Macías García F, Seijo Ríos S, Iglesias García J, Domínguez Muñoz JE. Pancreatitis and systemic lupus erythematosus. Rev Esp Enferm Dig. 2009;101:571-579. [Cited in This Article: ] |
| 32. | Makol A, Petri M. Pancreatitis in systemic lupus erythematosus: frequency and associated factors - a review of the Hopkins Lupus Cohort. J Rheumatol. 2010;37:341-345. [Cited in This Article: ] |
| 33. | Wang F, Wang NS, Zhao BH, Tang LQ. Acute pancreatitis as an initial symptom of systemic lupus erythematosus: a case report and review of the literature. World J Gastroenterol. 2005;11:4766-4768. [Cited in This Article: ] |
| 34. | Pascual-Ramos V, Duarte-Rojo A, Villa AR, Hernández-Cruz B, Alarcón-Segovia D, Alcocer-Varela J, Robles-Díaz G. Systemic lupus erythematosus as a cause and prognostic factor of acute pancreatitis. J Rheumatol. 2004;31:707-712. [Cited in This Article: ] |
| 35. | Gupta D, Mirza N. Systemic lupus erythematosus, celiac disease and antiphospholipid antibody syndrome: a rare association. Rheumatol Int. 2008;28:1179-1180. [Cited in This Article: ] |
| 36. | Hrycek A, Siekiera U. Coeliac disease in systemic lupus erythematosus: a case report. Rheumatol Int. 2008;28:491-493. [Cited in This Article: ] |
| 37. | Medeiros DA, Isenberg DA. Systemic lupus erythematosus and ulcerative colitis. Lupus. 2009;18:762-763. [Cited in This Article: ] |
| 38. | Su KY, Tsai ST, Tsay SH, Lee HT, Chen WS, Huang DF. A patient with systemic lupus erythematosus and Crohn's disease complicated with massive lower gastrointestinal bleeding, mimicking intestinal vasculitis. Lupus. 2008;17:1049-1050. [Cited in This Article: ] |
| 39. | Jaimes-Hernandez J, Aranda-Peirera P, Melendez-Mercado CI. Eosinophilic enteritis in association with systemic lupus erythematosus. Lupus. 2009;18:452-456. [Cited in This Article: ] |
| 40. | Mizoguchi F, Nanki T, Miyasaka N. Pneumatosis cystoides intestinalis following lupus enteritis and peritonitis. Intern Med. 2008;1267-1271. [Cited in This Article: ] |