-
PDF
- Split View
-
Views
-
Cite
Cite
Cheuk-Kit Wong, Ralph A.H. Stewart, Wanzhen Gao, John K. French, Christopher Raffel, Harvey D. White, for the Hirulog and Early Reperfusion or Occlusion (HERO-2) Trial Investigators, Prognostic differences between different types of bundle branch block during the early phase of acute myocardial infarction: insights from the Hirulog and Early Reperfusion or Occlusion (HERO)-2 trial, European Heart Journal, Volume 27, Issue 1, January 2006, Pages 21–28, https://doi.org/10.1093/eurheartj/ehi622
Close - Share Icon Share
Abstract
Aims Bundle branch block (BBB) early during acute myocardial infarction (AMI) is often considered high risk for mortality. Little is known about how different BBB types influence prognosis.
Methods and results The HERO-2 trial recruited 17 073 patients with ischaemic symptoms lasting >30 min and either ST elevation with or without right bundle branch block (RBBB) or presumed-new left bundle branch block (LBBB). Electrocardiograms were performed before and 60 min after the start of fibrinolytic therapy. Using patients with normal intraventricular conduction as a reference, odds ratios (ORs) for 30-day mortality were calculated for different BBB types (LBBB, RBBB with anterior AMI, and RBBB with inferior AMI) present at randomization and/or 60 min, with adjustment for recruitment region, pre-infarction characteristics, time to randomization, hemodynamics, and Killip class. At randomization, the 873 patients (5.11%) with BBB had worse baseline characteristics than patients without BBB. In patients presenting with LBBB (n=300), the ORs for 30-day mortality were 1.90 (95% CI 1.39–2.59) before and 0.68 (0.48–0.99) after adjustment for other prognosticators. In patients presenting with RBBB (n=415) and anterior AMI, the ORs were 3.52 (2.82–4.38) before and 2.48 (1.93–3.19) after adjustment. In patients presenting with RBBB and inferior AMI (n=158), the ORs were 1.74 (1.06–2.86) before and 1.22 (0.71–2.08) after adjustment. Within 60 min, 143 patients (0.92%) developed new BBB. The adjusted ORs for 30-day mortality were 2.97 (1.16–7.57) in the 25 patients with new LBBB, 3.84 (2.38–6.22) in the 100 with new RBBB and anterior AMI, and 2.23 (0.54–9.21) in the 18 with new RBBB and inferior AMI.
Conclusion RBBB accompanying anterior AMI at presentation and new BBB (including LBBB) early after fibrinolytic therapy are independent predictors of high 30-day mortality. These electrocardiographic features should be considered in risk stratification to identify high-risk patients.
See page 1 for the editorial comment on this article (doi:10.1093/eurheartj/ehi552)
Introduction
In the Fibrinolytic Therapy Trialists' meta-analysis, patients with bundle branch block (BBB) at randomization had a 35-day mortality rate of 23.6% without and 18.7% with fibrinolytic therapy.1 The trials included in the meta-analysis made no distinction between right bundle branch block (RBBB) and left bundle branch block (LBBB) and did not specify whether the BBB was new or old.1
Different types of BBB occurring during the initial hours of acute myocardial infarction (AMI) may have different prognostic implications that are independent of other prognostic factors. Development of new BBB despite prompt fibrinolytic therapy may signify an extensive and ongoing AMI.2 Some types of BBB may reflect larger infarct territories, indicating that these patients might benefit from more aggressive reperfusion therapy.
Current risk score algorithms, such as the thrombolysis in myocardial infarction (TIMI)3 and Global Utilization of Streptokinase and Tissue Plasminogen Activator for Occluded Coronary Arteries (GUSTO)4 risk scores, do not take RBBB into account, and only the TIMI score includes LBBB as a risk factor.
In the Hirulog and Early Reperfusion or Occlusion (HERO)-2 trial,5 which compared bivalirudin with unfractionated heparin in patients receiving fibrinolytic therapy for AMI, electrocardiograms (ECGs) were recorded at randomization and at 60 min after commencing fibrinolytic therapy. There was no difference in 30-day mortality between the two treatment groups. We evaluated the prognostic value of the three different types of BBB (LBBB, RBBB with anterior AMI, and RBBB with inferior AMI) present at these two timepoints.
Methods
The primary findings of the HERO-2 trial have been published elsewhere.5 Patients presenting with ischaemic chest pain lasting >30 min, ST elevation, or presumed-new LBBB within 6 h of symptom onset were given streptokinase and aspirin and randomized to receive either bivalirudin or unfractionated heparin. The primary endpoint was 30-day mortality.
This analysis was predefined prior to data lock in the HERO-2 trial. ECGs were performed at randomization and at 60 min after commencing fibrinolytic therapy. All ECGs were sent to the core electrocardiographic laboratory at Green Lane Hospital (Auckland, New Zealand) for analysis. A team of eight experienced electrocardiographic technicians screened the ECGs of all trial patients to identify those with any widening of the QRS complexes on any of the paired ECGs. Those ECGs were then reviewed by a cardiologist (CKW) to identify the current cohort who had BBB at either of the two timepoints. Inter-observer variability and intra-observer variability were not evaluated.
Definitions of LBBB and RBBB
LBBB was defined as the QRS duration of ≥0.12 s in the presence of sinus or supraventricular rhythm; a QS or rS complex in lead V1 or an R-wave peak time of ≥0.06 s (often with a notched R-wave) in lead I, AVL, V5, or V6 associated with the absence of a Q-wave in the same lead.6 RBBB was defined as a prolonged QRS duration of ≥0.12 s or an rsr', rsR', or rSR' pattern in lead V1 or V2. If this was not present, the R-wave in lead V1 had to be notched with a prolonged R-wave peak time of >0.05 s in lead V1 and a normal peak time in leads V5 and V6. Leads V6 and I had to show a QRS complex with a wide S-wave (S duration >R duration or >0.04 s).7
In the ECGs showing an RBBB pattern, ST-segment changes were measured at the J-point. AMI was classified as anterior if there was ≥2 mm of ST elevation in two contiguous leads between V1 and V3. AMI was classified as inferior if there was ≥1 mm of ST elevation in two contiguous leads between II, III, and AVF. Isolated ST elevation of ≥1 mm in two contiguous lateral leads between V4 and V6, I, and AVL was classified as anterior AMI. Patients with both anterior and inferior ST elevation were classified as having anterior AMI. Cases of RBBB (n=21) that did not fulfil any of these criteria were classified as anterior or inferior AMI depending on the location of the lead with the greatest ST elevation.
Assessment of clinical prognostic factors and peak enzyme levels
GUSTO risk scores were calculated to quantify the overall effect of various risk factors for 30-day mortality. This score is based on rated contributions from the interaction between age and Killip class, heart rate, systolic blood pressure, previous AMI, and AMI location.4 The peak enzyme level was expressed as multiples of the upper limit of normal (ULN) based on the creatine kinase myocardial band (CK-MB) level or the creatine kinase (CK) level, if the CK-MB level was unknown.
Statistical analysis
Data are presented as proportions or median values with interquartile ranges (IQRs) as appropriate. Comparisons between groups were done using χ2 tests for categorical variables and the Mann–Whitney U test for continuous variables. Comparisons were two-sided. P-values of <0.05 were considered significant. No adjustment was made for multiple comparisons.
Using patients with normal intraventricular conduction at both randomization and 60 min as a reference, the ORs for 24-h and 30-day mortality were calculated in patients with LBBB and RBBB at randomization. Data from patients with RBBB were analysed further according to the location of the AMI (anterior or inferior) and compared with data from patients who had normal conduction with AMI in the same location. The ORs were similarly calculated for new LBBB and new RBBB developing within 60 min after presentation with normal intraventricular conduction.
To determine whether different types of BBB had independent prognostic value, we calculated the OR for 30-day mortality in each BBB subgroup and performed multivariable logistic regression analysis to adjust stepwise for the different factors that might influence mortality. Randomization to bivalirudin or heparin did not influence 30-day mortality5 and was not a predictor in any multivariable modelling of the association between BBB and 30-day mortality.
The analysis was initially adjusted for the recruitment region (Russia, Eastern Europe, Western countries, Latin America, and Asia). Next, adjustments were made for pre-infarction characteristics including age, gender, previous AMI, previous coronary or vascular disease (including percutaneous coronary intervention, coronary artery bypass grafting, previous angina, stroke, and transient ischaemic attack), diabetes mellitus, and smoking. Further adjustment was made for the time to randomization. Finally, the models were adjusted for pulse rate, systolic blood pressure and Killip class. Mortality at 24 h was assessed as a secondary endpoint.8
Results
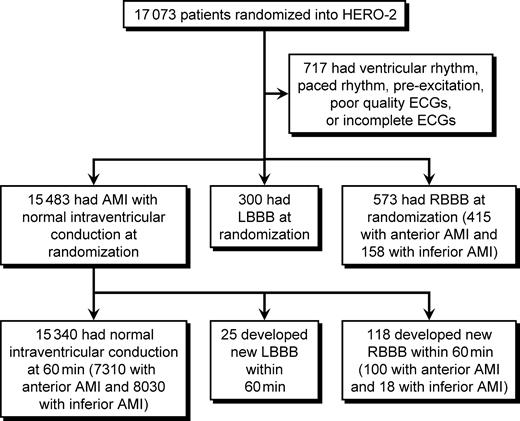
HERO-2 recruited 17 073 patients (Figure 1). BBB was present at randomization in 873 patients (5.11%) including 300 (1.76%) with LBBB and 573 (3.36%) with RBBB (415 with anterior AMI and 158 with inferior AMI). Of the 15 483 patients who had normal intraventricular conduction at randomization, 143 (0.92%) developed new BBB within 60 min after commencement of fibrinolytic therapy including new LBBB in 25 (0.16%) and new RBBB in 118 (0.76%; 100 with anterior AMI and 18 with inferior AMI). The remaining 15 340 patients had normal intraventricular conduction at both timepoints.
Among patients who had BBB at either of the two timepoints, the proportion of patients whose BBB developed newly within 60 min was higher among patients with RBBB accompanying anterior AMI (19.4%) than among those with RBBB accompanying inferior AMI (10.2%, P=0.005) and those with LBBB (7.7%, P<0.001).
The 30-day mortality rates in the different BBB groups ranged from 11.4% in patients presenting with RBBB accompanying inferior AMI to >30% in those developing new LBBB within 60 min and in those presenting with or developing new RBBB accompanying anterior AMI (Tables 1–3). Approximately 40% of deaths occurred within 24 h.
Patients with LBBB
Baseline characteristics were worse in the 300 patients with LBBB at randomization and in the 25 patients developing new LBBB within 60 min than in the 15 340 patients with normal intraventricular conduction at both timepoints (Table 1). The GUSTO risk scores were 61 (IQR 50–70) in patients with normal conduction, 74 (IQR 63–84) in those with LBBB at randomization (P<0.001), and 70 (IQR 63–78) in those developing new LBBB within 60 min (P<0.001).
The peak CK or CK-MB levels were higher in patients developing new LBBB within 60 min (10.8 times the ULN, IQR 6.3–21.3, P=0.03) than in those with normal conduction (7.5 times the ULN, IQR 3.4-14.1), but lower in those with LBBB at randomization (4.1 times the ULN, IQR 2.0–9.1, P<0.001).
The 30-day mortality rates ranged from 9.1% in patients with normal conduction to 16% in those with LBBB at randomization (P<0.001) and 32% in those developing new LBBB within 60 min (P<0.001).
Patients with RBBB accompanying anterior AMI
The 415 patients with RBBB accompanying anterior AMI at randomization had worse baseline characteristics than the 7310 patients with anterior MI and normal intraventricular conduction at both randomization and 60 min. The 100 patients who developed new RBBB within 60 min had similar baseline characteristics to those of patients with anterior AMI who did not develop RBBB (Table 2). The GUSTO risk scores were 65 (IQR 53–74) in patients with normal conduction, 72 (IQR 61–81) in those with RBBB at randomization (P<0.001), and 66.5 (IQR 57–76) in those developing new RBBB within 60 min (P=0.22).
The peak CK or CK-MB levels were higher in patients with RBBB at randomization (12.1 times the ULN, IQR 4.4–23.8, P<0.001) and in those developing new RBBB within 60 min (16.6 times the ULN, IQR 8.9–24.0, P<0.001) than in those with normal conduction (7.6 times the ULN, IQR 3.1–14.9).
Similarly, the 30-day mortality rates were higher in patients with RBBB at randomization (31.6%, P<0.001) and in those developing new RBBB within 60 min (33%, P<0.001) than in those with normal conduction (11.6%).
Patients with RBBB accompanying inferior AMI
Baseline characteristics were worse in the 158 patients with RBBB accompanying inferior AMI at randomization and in the 18 patients developing new RBBB within 60 min than in the 8030 patients with normal intraventricular conduction at both timepoints (Table 3). The GUSTO risk scores were 55 (IQR 46–66) in patients with normal conduction, 65 (IQR 55–74) in those with RBBB at randomization (P<0.001), and 61 (IQR 55–76) in those developing new RBBB within 60 min (P=0.03).
The peak CK or CK-MB levels were 7.4 times the ULN (IQR 3.7–13.4) in patients with normal conduction, 6.3 times the ULN (IQR 2.8–12.6, P=0.15) in those with RBBB at randomization, and 11.6 times the ULN (IQR 5.3–14.0, P=0.47) in those developing new RBBB within 60 min.
The 30-day mortality rates were 6.9% in patients with normal conduction, 11.4% in those with RBBB at randomization (P=0.03), and 16.7% in those developing new RBBB within 60 min (P=0.12).
Adjusted 30-day mortality
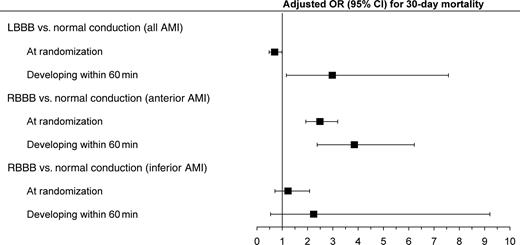
Table 4 shows the ORs for 30-day mortality before and after each adjustment step, when compared with the reference groups. In patients with LBBB at randomization, the unadjusted OR was 1.90 (95% CI 1.39–2.59), decreasing to 1.10 (95% CI 0.79–1.53) after adjustment for pre-infarction characteristics and to 0.69 (95% CI 0.48–0.99) after further adjustment for the presenting features of AMI. In contrast, the OR was significantly increased in patients developing new LBBB within 60 min, both before (4.68, 95% CI 2.02–10.87) and after all adjustments (2.97, 95% CI 1.16–7.57) (Figure 2).
Patients with RBBB accompanying anterior AMI at randomization had a significantly increased OR for 30-day mortality of 3.52 (95% CI 2.82–4.38) before adjustment, 3.24 (95% CI 2.55–4.11) after adjustment for pre-infarction characteristics, and 2.48 (95% CI 1.93–3.19) after further adjustment for the presenting features of AMI. In patients who developed new RBBB within 60 min, the OR was also significantly increased both before (3.75, 95% CI 2.46–5.73) and after all adjustments (3.84, 95% CI 2.38–6.22) (Figure 2). Analysis using 24-h mortality as the endpoint yielded similar results.
In patients with RBBB accompanying inferior AMI at randomization, the ORs for 30-day mortality were 1.74 (95% CI 1.06–2.86) before adjustment, 1.21 (95% CI 0.72–2.03) after adjustment for pre-infarction characteristics, and 1.22 (95% CI 0.71–2.08) after further adjustment for the presenting features of AMI. In patients developing new RBBB within 60 min, the ORs were 2.71 (95% CI 0.78–9.38) before and 2.23 (95% CI 0.54–9.21) after all adjustments (Figure 2).
Discussion
This report describes a prospective series of 1016 patients with BBB early during AMI, with 30-day mortality rates ranging from 11.4 to >30%. Patients with any type of BBB at randomization had worse baseline characteristics than those with normal intraventricular conduction. However, only patients with RBBB accompanying anterior AMI at randomization (and not patients with RBBB accompanying inferior AMI or patients with LBBB at randomization) had a higher mortality rate after adjustment for baseline characteristics. This finding persisted after further adjustment for the presenting features of AMI.
Approximately 1% of patients who had ST-elevation AMI with normal intraventricular conduction at randomization developed new BBB (most commonly RBBB accompanying anterior AMI) within 60 min after commencing fibrinolytic therapy. New BBB was associated with higher 30-day mortality.
The higher mortality and the higher incidence of RBBB seen in patients with anterior AMI may be explained by septal ischaemia from a more proximal left anterior descending artery occlusion (before the large septal branch) and the course of the right bundle branch traversing the septum towards the apex. Higher peak enzyme levels were observed in these patients. In contrast, the left bundle has a more varied distribution from a true bifascicular system to a network of fibres,9 and more extensive ischaemia or necrosis is required to produce complete LBBB. Thus, new LBBB was far less likely to develop within 60 min than new RBBB, but when new LBBB did develop, the mortality rate was as high as that of patients with RBBB accompanying anterior AMI.
In the current American10 and European guidelines,11 new or presumed-new LBBB within 12 h after the onset of symptoms suggestive of AMI is a Class I indication for fibrinolytic therapy. New or presumed-new LBBB was an inclusion criterion in the HERO-2 trial. The 300 HERO-2 patients with LBBB at randomization had worse pre-infarction characteristics (older age and previous AMI), worse presenting features (higher pulse rate and Killip class), and nearly twice the unadjusted 30-day mortality rate of patients with normal conduction. However, after adjustment for pre-infarction characteristics and presenting features, their 30-day mortality rate was no higher than that of patients with normal intraventricular conduction12—an interesting observation which corroborates the findings of a GUSTO-1 substudy in 131 patients with LBBB.13
Of the 300 HERO-2 patients with LBBB at randomization (1.76% of the total HERO-2 cohort), 80% had enzymatic evidence of AMI. This rate is 10% lower than that of patients with normal intraventricular conduction,12 which may partly explain the relatively good outcome of these 300 patients. There can be wide heterogeneity among patients presenting with LBBB and chest pain, as demonstrated by community studies in which as few as 13% of patients presenting with LBBB had enzymatic evidence of AMI.14,15
In contrast to the relatively good prognosis of patients with LBBB at randomization, the 30-day mortality rate of patients developing LBBB within 60 min after presenting with normal conduction trebled after similar adjustment steps. The development of new LBBB in these patients was probably due to extensive ongoing AMI,2 considering that the patients all had ST-elevation AMI before developing LBBB and had larger infarcts (as judged by enzymatic criteria) than patients with LBBB at randomization.
Clinical implications
The current study demonstrates a means of early identification of patient subgroups with particular BBB characteristics that are independently associated with higher 30-day mortality. These electrocardiographic features add important prognostic information that supplements the clinical parameters commonly used in early risk stratification algorithms.3,4 Our secondary analysis confirmed that patients with RBBB accompanying anterior AMI had higher mortality not only at 30 days but also at 24 h. The mortality rates we observed were similar to those reported previously.2,13,16–21
By performing serial early electrocardiographic recordings, the current study is unique in comparing LBBB at presentation with new LBBB developing subsequent to presentation with normal conduction. Although patients presenting with LBBB (which was judged to be new by the study investigators) had a higher overall mortality rate than patients with normal intraventricular conduction, this was mainly because they had worse pre-infarction characteristics including older age.
In-hospital revascularization was relatively uncommon in HERO-2, as shown in Tables 1–3. Although the Grupo de Análisis de la Cardiopatía Isquémica Aguda trial recently reported benefits at 1 year from early revascularization after fibrinolytic therapy for ST-elevation AMI, no benefit was evident at 30 days.22 Analysis of the contemporary Global Registry of Acute Coronary Events registry showed that access to catheterization facilities did not influence mortality (12.4 vs. 12.4%) or non-fatal AMI rates (3.3% with access vs. 3.6% without access) at 6 months.23 There is also controversy about the benefit of rescue intervention, although in the Middlesbrough Early Revascularization to Limit Infarction trial of 307 patients with failed fibrinolysis, there was a trend towards decreased 30-day mortality in patients who had rescue percutaneous coronary intervention (9.8 vs. 11%, P=0.07).24
Our finding that 30-day mortality trebled to >30% in patients who presented with RBBB accompanying anterior AMI or who developed new BBB despite fibrinolytic therapy suggests that such patients may benefit from more aggressive reperfusion therapy. The benefit of emergency revascularization has previously been demonstrated in patients with cardiogenic shock,25 and future studies should evaluate whether this also holds true for very high-risk BBB patients.
Limitations
As in all clinical trials, a selection bias could have occurred in HERO-2 resulting in under-representation of very high-risk patients (including those with RBBB accompanying anterior AMI) in the trial cohort.
Conclusions
Patients who have RBBB accompanying anterior AMI at presentation or who develop new BBB early after fibrinolytic therapy independently have higher 30-day mortality than patients without these conduction abnormalities. Patients with LBBB at presentation do not have increased mortality after adjustment for their worse baseline characteristics. These electrocardiographic features add important prognostic information that supplements the clinical parameters commonly used in early risk stratification algorithms.
Acknowledgements
The authors would like to thank many investigators and patients who participated in the HERO-2 trial; Maggie Scott, RGON, who was global project manager for the trial; Teena West, MSc, for statistical advice; Barbara Semb for secretarial assistance; and Anna Breckon, ELS, for editorial assistance. H.D.W. received partial salary support from the Green Lane Research and Educational Fund Board (Auckland, New Zealand).
Conflict of interest: none declared.
Figure 1 Flow chart of patients in the HERO-2 trial.
Figure 2 Adjusted ORs and 95% CI for 30-day mortality in the different categories of BBB present at randomization and the different categories of new BBB developing within 60 min after commencement of fibrinolytic therapy.
Table 1 Baseline characteristics and mortality in patients with LBBB vs. normal intraventricular conduction
| . | Normal conduction at randomization and 60 min (n=15 340) . | LBBB at randomization (n=300) . | P-value . | New LBBB developing within 60 min (n=25) . | P-value . |
|---|---|---|---|---|---|
| Demographics | |||||
| Age (years)a | 61 (51–70) | 68.5 (61–75) | <0.001 | 67 (60–75) | 0.006 |
| Age ≥75 years (%) | 12 | 26 | <0.001 | 28 | 0.024 |
| Women (%) | 28.2 | 43 | <0.001 | 48 | 0.028 |
| Previous cardiovascular disease and interventions (%) | |||||
| Angina | 46.5 | 62.7 | <0.001 | 64 | 0.079 |
| AMI | 14.5 | 30.7 | <0.001 | 20 | 0.395 |
| Percutaneous coronary intervention | 1.2 | 0.3 | 0.277 | 4 | 0.268 |
| Coronary artery bypass grafting | 0.7 | 0 | 0.285 | 0 | 1.0 |
| Cardiovascular risk factors (%) | |||||
| Smoking history (%) | |||||
| Never smoked | 38.3 | 51.3 | <0.001 | 48 | 0.575 |
| Past smoking | 44.8 | 27.3 | 40 | ||
| Current smoking | 17 | 21.3 | 12 | ||
| Hypertension | 51.3 | 68.7 | <0.001 | 64 | 0.205 |
| Diabetes | 13.7 | 17 | 0.099 | 48 | <0.001 |
| Time from symptom onset to randomization (h)a | 3.1 (2.2–4.2) | 3.4 (2.4–4.2) | 0.016 | 2.6 (1.8–3.4) | 0.038 |
| Hemodynamics | |||||
| Systolic blood pressure (mmHg)a | 135 (120–150) | 140 (120–160) | 0.057 | 135 (110–155) | 0.697 |
| Heart rate (beats/minute)a | 76 (65–88) | 88 (75–101) | <0.001 | 74 (62–90) | 0.778 |
| Killip Class (%) | |||||
| I | 80.1 | 54.3 | <0.001 | 60 | 0.028 |
| II | 16.7 | 26.7 | 32 | ||
| III | 2.1 | 16 | 8 | ||
| IV | 1.1 | 3 | 0 | ||
| Randomization to bivalirudin (%) | 49.9 | 49.3 | 0.837 | 56 | |
| GUSTO risk scorea | 61 (50–70) | 74 (63–84) | <0.001 | 70 (63–78) | 0.001 |
| Peak enzyme level expressed as multiple of ULNa,b | 7.5 (3.4–14.1) | 4.1 (2.0–9.1) | <0.001 | 10.8 (6.3–21.3) | 0.035 |
| In-hospital revascularization (%) | |||||
| Percutaneous coronary intervention | 5.7 | 2.7 | 0.026 | 12.0 | 0.167 |
| Coronary artery bypass grafting | 0.7 | 1.3 | 0.286 | 8.0 | 0.015 |
| Mortality (%) | |||||
| Within 30 days | 9.1 | 16 | <0.001 | 32 | 0.001 |
| Within 24 h | 3.5 | 6.7 | 0.004 | 8 | 0.219 |
| . | Normal conduction at randomization and 60 min (n=15 340) . | LBBB at randomization (n=300) . | P-value . | New LBBB developing within 60 min (n=25) . | P-value . |
|---|---|---|---|---|---|
| Demographics | |||||
| Age (years)a | 61 (51–70) | 68.5 (61–75) | <0.001 | 67 (60–75) | 0.006 |
| Age ≥75 years (%) | 12 | 26 | <0.001 | 28 | 0.024 |
| Women (%) | 28.2 | 43 | <0.001 | 48 | 0.028 |
| Previous cardiovascular disease and interventions (%) | |||||
| Angina | 46.5 | 62.7 | <0.001 | 64 | 0.079 |
| AMI | 14.5 | 30.7 | <0.001 | 20 | 0.395 |
| Percutaneous coronary intervention | 1.2 | 0.3 | 0.277 | 4 | 0.268 |
| Coronary artery bypass grafting | 0.7 | 0 | 0.285 | 0 | 1.0 |
| Cardiovascular risk factors (%) | |||||
| Smoking history (%) | |||||
| Never smoked | 38.3 | 51.3 | <0.001 | 48 | 0.575 |
| Past smoking | 44.8 | 27.3 | 40 | ||
| Current smoking | 17 | 21.3 | 12 | ||
| Hypertension | 51.3 | 68.7 | <0.001 | 64 | 0.205 |
| Diabetes | 13.7 | 17 | 0.099 | 48 | <0.001 |
| Time from symptom onset to randomization (h)a | 3.1 (2.2–4.2) | 3.4 (2.4–4.2) | 0.016 | 2.6 (1.8–3.4) | 0.038 |
| Hemodynamics | |||||
| Systolic blood pressure (mmHg)a | 135 (120–150) | 140 (120–160) | 0.057 | 135 (110–155) | 0.697 |
| Heart rate (beats/minute)a | 76 (65–88) | 88 (75–101) | <0.001 | 74 (62–90) | 0.778 |
| Killip Class (%) | |||||
| I | 80.1 | 54.3 | <0.001 | 60 | 0.028 |
| II | 16.7 | 26.7 | 32 | ||
| III | 2.1 | 16 | 8 | ||
| IV | 1.1 | 3 | 0 | ||
| Randomization to bivalirudin (%) | 49.9 | 49.3 | 0.837 | 56 | |
| GUSTO risk scorea | 61 (50–70) | 74 (63–84) | <0.001 | 70 (63–78) | 0.001 |
| Peak enzyme level expressed as multiple of ULNa,b | 7.5 (3.4–14.1) | 4.1 (2.0–9.1) | <0.001 | 10.8 (6.3–21.3) | 0.035 |
| In-hospital revascularization (%) | |||||
| Percutaneous coronary intervention | 5.7 | 2.7 | 0.026 | 12.0 | 0.167 |
| Coronary artery bypass grafting | 0.7 | 1.3 | 0.286 | 8.0 | 0.015 |
| Mortality (%) | |||||
| Within 30 days | 9.1 | 16 | <0.001 | 32 | 0.001 |
| Within 24 h | 3.5 | 6.7 | 0.004 | 8 | 0.219 |
aMedian (interquartile range).
bThe peak enzyme level was based on the CK-MB level where available or on the CK level if the CK-MB level was not available.
Table 1 Baseline characteristics and mortality in patients with LBBB vs. normal intraventricular conduction
| . | Normal conduction at randomization and 60 min (n=15 340) . | LBBB at randomization (n=300) . | P-value . | New LBBB developing within 60 min (n=25) . | P-value . |
|---|---|---|---|---|---|
| Demographics | |||||
| Age (years)a | 61 (51–70) | 68.5 (61–75) | <0.001 | 67 (60–75) | 0.006 |
| Age ≥75 years (%) | 12 | 26 | <0.001 | 28 | 0.024 |
| Women (%) | 28.2 | 43 | <0.001 | 48 | 0.028 |
| Previous cardiovascular disease and interventions (%) | |||||
| Angina | 46.5 | 62.7 | <0.001 | 64 | 0.079 |
| AMI | 14.5 | 30.7 | <0.001 | 20 | 0.395 |
| Percutaneous coronary intervention | 1.2 | 0.3 | 0.277 | 4 | 0.268 |
| Coronary artery bypass grafting | 0.7 | 0 | 0.285 | 0 | 1.0 |
| Cardiovascular risk factors (%) | |||||
| Smoking history (%) | |||||
| Never smoked | 38.3 | 51.3 | <0.001 | 48 | 0.575 |
| Past smoking | 44.8 | 27.3 | 40 | ||
| Current smoking | 17 | 21.3 | 12 | ||
| Hypertension | 51.3 | 68.7 | <0.001 | 64 | 0.205 |
| Diabetes | 13.7 | 17 | 0.099 | 48 | <0.001 |
| Time from symptom onset to randomization (h)a | 3.1 (2.2–4.2) | 3.4 (2.4–4.2) | 0.016 | 2.6 (1.8–3.4) | 0.038 |
| Hemodynamics | |||||
| Systolic blood pressure (mmHg)a | 135 (120–150) | 140 (120–160) | 0.057 | 135 (110–155) | 0.697 |
| Heart rate (beats/minute)a | 76 (65–88) | 88 (75–101) | <0.001 | 74 (62–90) | 0.778 |
| Killip Class (%) | |||||
| I | 80.1 | 54.3 | <0.001 | 60 | 0.028 |
| II | 16.7 | 26.7 | 32 | ||
| III | 2.1 | 16 | 8 | ||
| IV | 1.1 | 3 | 0 | ||
| Randomization to bivalirudin (%) | 49.9 | 49.3 | 0.837 | 56 | |
| GUSTO risk scorea | 61 (50–70) | 74 (63–84) | <0.001 | 70 (63–78) | 0.001 |
| Peak enzyme level expressed as multiple of ULNa,b | 7.5 (3.4–14.1) | 4.1 (2.0–9.1) | <0.001 | 10.8 (6.3–21.3) | 0.035 |
| In-hospital revascularization (%) | |||||
| Percutaneous coronary intervention | 5.7 | 2.7 | 0.026 | 12.0 | 0.167 |
| Coronary artery bypass grafting | 0.7 | 1.3 | 0.286 | 8.0 | 0.015 |
| Mortality (%) | |||||
| Within 30 days | 9.1 | 16 | <0.001 | 32 | 0.001 |
| Within 24 h | 3.5 | 6.7 | 0.004 | 8 | 0.219 |
| . | Normal conduction at randomization and 60 min (n=15 340) . | LBBB at randomization (n=300) . | P-value . | New LBBB developing within 60 min (n=25) . | P-value . |
|---|---|---|---|---|---|
| Demographics | |||||
| Age (years)a | 61 (51–70) | 68.5 (61–75) | <0.001 | 67 (60–75) | 0.006 |
| Age ≥75 years (%) | 12 | 26 | <0.001 | 28 | 0.024 |
| Women (%) | 28.2 | 43 | <0.001 | 48 | 0.028 |
| Previous cardiovascular disease and interventions (%) | |||||
| Angina | 46.5 | 62.7 | <0.001 | 64 | 0.079 |
| AMI | 14.5 | 30.7 | <0.001 | 20 | 0.395 |
| Percutaneous coronary intervention | 1.2 | 0.3 | 0.277 | 4 | 0.268 |
| Coronary artery bypass grafting | 0.7 | 0 | 0.285 | 0 | 1.0 |
| Cardiovascular risk factors (%) | |||||
| Smoking history (%) | |||||
| Never smoked | 38.3 | 51.3 | <0.001 | 48 | 0.575 |
| Past smoking | 44.8 | 27.3 | 40 | ||
| Current smoking | 17 | 21.3 | 12 | ||
| Hypertension | 51.3 | 68.7 | <0.001 | 64 | 0.205 |
| Diabetes | 13.7 | 17 | 0.099 | 48 | <0.001 |
| Time from symptom onset to randomization (h)a | 3.1 (2.2–4.2) | 3.4 (2.4–4.2) | 0.016 | 2.6 (1.8–3.4) | 0.038 |
| Hemodynamics | |||||
| Systolic blood pressure (mmHg)a | 135 (120–150) | 140 (120–160) | 0.057 | 135 (110–155) | 0.697 |
| Heart rate (beats/minute)a | 76 (65–88) | 88 (75–101) | <0.001 | 74 (62–90) | 0.778 |
| Killip Class (%) | |||||
| I | 80.1 | 54.3 | <0.001 | 60 | 0.028 |
| II | 16.7 | 26.7 | 32 | ||
| III | 2.1 | 16 | 8 | ||
| IV | 1.1 | 3 | 0 | ||
| Randomization to bivalirudin (%) | 49.9 | 49.3 | 0.837 | 56 | |
| GUSTO risk scorea | 61 (50–70) | 74 (63–84) | <0.001 | 70 (63–78) | 0.001 |
| Peak enzyme level expressed as multiple of ULNa,b | 7.5 (3.4–14.1) | 4.1 (2.0–9.1) | <0.001 | 10.8 (6.3–21.3) | 0.035 |
| In-hospital revascularization (%) | |||||
| Percutaneous coronary intervention | 5.7 | 2.7 | 0.026 | 12.0 | 0.167 |
| Coronary artery bypass grafting | 0.7 | 1.3 | 0.286 | 8.0 | 0.015 |
| Mortality (%) | |||||
| Within 30 days | 9.1 | 16 | <0.001 | 32 | 0.001 |
| Within 24 h | 3.5 | 6.7 | 0.004 | 8 | 0.219 |
aMedian (interquartile range).
bThe peak enzyme level was based on the CK-MB level where available or on the CK level if the CK-MB level was not available.
Table 2 Baseline characteristics and mortality in patients who had anterior AMI with RBBB versus anterior AMI with normal intraventricular conduction
| . | Anterior AMI with normal conduction at randomization and 60 min (n=7310) . | Anterior AMI with RBBB at randomization (n=415) . | P-value . | Anterior AMI with new RBBB developing within 60 min (n=100) . | P-value . |
|---|---|---|---|---|---|
| Demographics | |||||
| Age (years)a | 62 (51–70) | 66 (56–73) | <0.001 | 62 (52–69.5) | 0.868 |
| Age ≥75 years (%) | 12.7 | 19.5 | <0.001 | 12 | 0.839 |
| Women (%) | 28.7 | 26 | 0.247 | 36 | 0.107 |
| Previous cardiovascular disease and interventions (%) | |||||
| Angina | 49.9 | 51.1 | 0.644 | 52 | 0.679 |
| AMI | 15.8 | 16.6 | 0.632 | 15 | 0.839 |
| Percutaneous coronary intervention | 1.0 | 0.7 | 0.798 | 1 | 1.0 |
| Coronary artery bypass grafting | 0.5 | 1.5 | 0.029 | 0 | 1.0 |
| Cardiovascular risk factors (%) | |||||
| Smoking history (%) | |||||
| Never smoked | 41 | 43.4 | 0.003 | 48 | 0.368 |
| Past smoking | 16.5 | 21.7 | 37 | ||
| Current smoking | 42.5 | 34.9 | 15 | ||
| Hypertension | 52.6 | 53.7 | 0.664 | 62 | 0.063 |
| Diabetes | 13.4 | 19 | 0.001 | 16 | 0.442 |
| Time from symptom onset to randomization (h)a | 3.2 (2.3–4.3) | 3.2 (2.1–4.2) | 0.647 | 2.8 (2.1–3.9) | 0.047 |
| Hemodynamics | |||||
| Systolic blood pressure (mmHg)a | 140 (120–150) | 130 (110–140) | <0.001 | 130 (110–140) | <0.001 |
| Heart rate (beats/min)a | 80 (70–90) | 85 (72–98) | <0.001 | 80 (68.5–89.5) | 0.820 |
| Killip Class (%) | |||||
| I | 76.4 | 63.1 | <0.001 | 70 | 0.172 |
| II | 19.7 | 27.7 | 22 | ||
| III | 2.9 | 4.3 | 6 | ||
| IV | 1 | 4.8 | 2 | ||
| Randomization to bivalirudin (%) | 50.5 | 49.6 | 0.739 | 50 | 0.924 |
| GUSTO risk scorea | 65 (53–74) | 72 (61–81) | <0.001 | 66.5 (57–76) | 0.220 |
| Peak enzyme level expressed as multiple of ULNa,b | 7.6 (3.1–14.9) | 12.1 (4.4–23.8) | <0.001 | 16.6 (8.6–24.0) | <0.001 |
| In-hospital revascularization (%) | |||||
| Percutaneous coronary intervention | 4.8 | 3.1 | 0.123 | 3 | 0.632 |
| Coronary artery bypass grafting | 0.6 | 0.2 | 0.729 | 0 | 1.0 |
| Mortality (%) | |||||
| Within 30 days | 11.6 | 31.6 | <0.001 | 33 | <0.001 |
| Within 24 h | 4.6 | 16.9 | <0.001 | 18 | <0.001 |
| . | Anterior AMI with normal conduction at randomization and 60 min (n=7310) . | Anterior AMI with RBBB at randomization (n=415) . | P-value . | Anterior AMI with new RBBB developing within 60 min (n=100) . | P-value . |
|---|---|---|---|---|---|
| Demographics | |||||
| Age (years)a | 62 (51–70) | 66 (56–73) | <0.001 | 62 (52–69.5) | 0.868 |
| Age ≥75 years (%) | 12.7 | 19.5 | <0.001 | 12 | 0.839 |
| Women (%) | 28.7 | 26 | 0.247 | 36 | 0.107 |
| Previous cardiovascular disease and interventions (%) | |||||
| Angina | 49.9 | 51.1 | 0.644 | 52 | 0.679 |
| AMI | 15.8 | 16.6 | 0.632 | 15 | 0.839 |
| Percutaneous coronary intervention | 1.0 | 0.7 | 0.798 | 1 | 1.0 |
| Coronary artery bypass grafting | 0.5 | 1.5 | 0.029 | 0 | 1.0 |
| Cardiovascular risk factors (%) | |||||
| Smoking history (%) | |||||
| Never smoked | 41 | 43.4 | 0.003 | 48 | 0.368 |
| Past smoking | 16.5 | 21.7 | 37 | ||
| Current smoking | 42.5 | 34.9 | 15 | ||
| Hypertension | 52.6 | 53.7 | 0.664 | 62 | 0.063 |
| Diabetes | 13.4 | 19 | 0.001 | 16 | 0.442 |
| Time from symptom onset to randomization (h)a | 3.2 (2.3–4.3) | 3.2 (2.1–4.2) | 0.647 | 2.8 (2.1–3.9) | 0.047 |
| Hemodynamics | |||||
| Systolic blood pressure (mmHg)a | 140 (120–150) | 130 (110–140) | <0.001 | 130 (110–140) | <0.001 |
| Heart rate (beats/min)a | 80 (70–90) | 85 (72–98) | <0.001 | 80 (68.5–89.5) | 0.820 |
| Killip Class (%) | |||||
| I | 76.4 | 63.1 | <0.001 | 70 | 0.172 |
| II | 19.7 | 27.7 | 22 | ||
| III | 2.9 | 4.3 | 6 | ||
| IV | 1 | 4.8 | 2 | ||
| Randomization to bivalirudin (%) | 50.5 | 49.6 | 0.739 | 50 | 0.924 |
| GUSTO risk scorea | 65 (53–74) | 72 (61–81) | <0.001 | 66.5 (57–76) | 0.220 |
| Peak enzyme level expressed as multiple of ULNa,b | 7.6 (3.1–14.9) | 12.1 (4.4–23.8) | <0.001 | 16.6 (8.6–24.0) | <0.001 |
| In-hospital revascularization (%) | |||||
| Percutaneous coronary intervention | 4.8 | 3.1 | 0.123 | 3 | 0.632 |
| Coronary artery bypass grafting | 0.6 | 0.2 | 0.729 | 0 | 1.0 |
| Mortality (%) | |||||
| Within 30 days | 11.6 | 31.6 | <0.001 | 33 | <0.001 |
| Within 24 h | 4.6 | 16.9 | <0.001 | 18 | <0.001 |
aMedian (interquartile range).
bThe peak enzyme level was based on the CK-MB level where available or on the CK level if the CK-MB level was not available.
Table 2 Baseline characteristics and mortality in patients who had anterior AMI with RBBB versus anterior AMI with normal intraventricular conduction
| . | Anterior AMI with normal conduction at randomization and 60 min (n=7310) . | Anterior AMI with RBBB at randomization (n=415) . | P-value . | Anterior AMI with new RBBB developing within 60 min (n=100) . | P-value . |
|---|---|---|---|---|---|
| Demographics | |||||
| Age (years)a | 62 (51–70) | 66 (56–73) | <0.001 | 62 (52–69.5) | 0.868 |
| Age ≥75 years (%) | 12.7 | 19.5 | <0.001 | 12 | 0.839 |
| Women (%) | 28.7 | 26 | 0.247 | 36 | 0.107 |
| Previous cardiovascular disease and interventions (%) | |||||
| Angina | 49.9 | 51.1 | 0.644 | 52 | 0.679 |
| AMI | 15.8 | 16.6 | 0.632 | 15 | 0.839 |
| Percutaneous coronary intervention | 1.0 | 0.7 | 0.798 | 1 | 1.0 |
| Coronary artery bypass grafting | 0.5 | 1.5 | 0.029 | 0 | 1.0 |
| Cardiovascular risk factors (%) | |||||
| Smoking history (%) | |||||
| Never smoked | 41 | 43.4 | 0.003 | 48 | 0.368 |
| Past smoking | 16.5 | 21.7 | 37 | ||
| Current smoking | 42.5 | 34.9 | 15 | ||
| Hypertension | 52.6 | 53.7 | 0.664 | 62 | 0.063 |
| Diabetes | 13.4 | 19 | 0.001 | 16 | 0.442 |
| Time from symptom onset to randomization (h)a | 3.2 (2.3–4.3) | 3.2 (2.1–4.2) | 0.647 | 2.8 (2.1–3.9) | 0.047 |
| Hemodynamics | |||||
| Systolic blood pressure (mmHg)a | 140 (120–150) | 130 (110–140) | <0.001 | 130 (110–140) | <0.001 |
| Heart rate (beats/min)a | 80 (70–90) | 85 (72–98) | <0.001 | 80 (68.5–89.5) | 0.820 |
| Killip Class (%) | |||||
| I | 76.4 | 63.1 | <0.001 | 70 | 0.172 |
| II | 19.7 | 27.7 | 22 | ||
| III | 2.9 | 4.3 | 6 | ||
| IV | 1 | 4.8 | 2 | ||
| Randomization to bivalirudin (%) | 50.5 | 49.6 | 0.739 | 50 | 0.924 |
| GUSTO risk scorea | 65 (53–74) | 72 (61–81) | <0.001 | 66.5 (57–76) | 0.220 |
| Peak enzyme level expressed as multiple of ULNa,b | 7.6 (3.1–14.9) | 12.1 (4.4–23.8) | <0.001 | 16.6 (8.6–24.0) | <0.001 |
| In-hospital revascularization (%) | |||||
| Percutaneous coronary intervention | 4.8 | 3.1 | 0.123 | 3 | 0.632 |
| Coronary artery bypass grafting | 0.6 | 0.2 | 0.729 | 0 | 1.0 |
| Mortality (%) | |||||
| Within 30 days | 11.6 | 31.6 | <0.001 | 33 | <0.001 |
| Within 24 h | 4.6 | 16.9 | <0.001 | 18 | <0.001 |
| . | Anterior AMI with normal conduction at randomization and 60 min (n=7310) . | Anterior AMI with RBBB at randomization (n=415) . | P-value . | Anterior AMI with new RBBB developing within 60 min (n=100) . | P-value . |
|---|---|---|---|---|---|
| Demographics | |||||
| Age (years)a | 62 (51–70) | 66 (56–73) | <0.001 | 62 (52–69.5) | 0.868 |
| Age ≥75 years (%) | 12.7 | 19.5 | <0.001 | 12 | 0.839 |
| Women (%) | 28.7 | 26 | 0.247 | 36 | 0.107 |
| Previous cardiovascular disease and interventions (%) | |||||
| Angina | 49.9 | 51.1 | 0.644 | 52 | 0.679 |
| AMI | 15.8 | 16.6 | 0.632 | 15 | 0.839 |
| Percutaneous coronary intervention | 1.0 | 0.7 | 0.798 | 1 | 1.0 |
| Coronary artery bypass grafting | 0.5 | 1.5 | 0.029 | 0 | 1.0 |
| Cardiovascular risk factors (%) | |||||
| Smoking history (%) | |||||
| Never smoked | 41 | 43.4 | 0.003 | 48 | 0.368 |
| Past smoking | 16.5 | 21.7 | 37 | ||
| Current smoking | 42.5 | 34.9 | 15 | ||
| Hypertension | 52.6 | 53.7 | 0.664 | 62 | 0.063 |
| Diabetes | 13.4 | 19 | 0.001 | 16 | 0.442 |
| Time from symptom onset to randomization (h)a | 3.2 (2.3–4.3) | 3.2 (2.1–4.2) | 0.647 | 2.8 (2.1–3.9) | 0.047 |
| Hemodynamics | |||||
| Systolic blood pressure (mmHg)a | 140 (120–150) | 130 (110–140) | <0.001 | 130 (110–140) | <0.001 |
| Heart rate (beats/min)a | 80 (70–90) | 85 (72–98) | <0.001 | 80 (68.5–89.5) | 0.820 |
| Killip Class (%) | |||||
| I | 76.4 | 63.1 | <0.001 | 70 | 0.172 |
| II | 19.7 | 27.7 | 22 | ||
| III | 2.9 | 4.3 | 6 | ||
| IV | 1 | 4.8 | 2 | ||
| Randomization to bivalirudin (%) | 50.5 | 49.6 | 0.739 | 50 | 0.924 |
| GUSTO risk scorea | 65 (53–74) | 72 (61–81) | <0.001 | 66.5 (57–76) | 0.220 |
| Peak enzyme level expressed as multiple of ULNa,b | 7.6 (3.1–14.9) | 12.1 (4.4–23.8) | <0.001 | 16.6 (8.6–24.0) | <0.001 |
| In-hospital revascularization (%) | |||||
| Percutaneous coronary intervention | 4.8 | 3.1 | 0.123 | 3 | 0.632 |
| Coronary artery bypass grafting | 0.6 | 0.2 | 0.729 | 0 | 1.0 |
| Mortality (%) | |||||
| Within 30 days | 11.6 | 31.6 | <0.001 | 33 | <0.001 |
| Within 24 h | 4.6 | 16.9 | <0.001 | 18 | <0.001 |
aMedian (interquartile range).
bThe peak enzyme level was based on the CK-MB level where available or on the CK level if the CK-MB level was not available.
Table 3 Baseline characteristics and mortality in patients who had inferior AMI with RBBB vs. inferior AMI with normal intraventricular conduction
| . | Inferior AMI with normal conduction at randomization and 60 min (n=8030) . | Inferior AMI with RBBB at randomization (n=158) . | P-value . | Inferior AMI with new RBBB developing within 60 min (n=18) . | P-value . |
|---|---|---|---|---|---|
| Demographics | |||||
| Age (years)a | 60 (51–69) | 68 (60–74) | <0.001 | 65 (59–70) | 0.079 |
| Age ≥75 years (%) | 11.4 | 23.4 | <0.001 | 11.1 | 1.0 |
| Women (%) | 27.8 | 21.5 | 0.080 | 11.1 | 0.114 |
| Previous cardiovascular disease and interventions (%) | |||||
| Angina | 43.3 | 49.4 | 0.128 | 33.3 | 0.394 |
| AMI | 13.4 | 22.8 | 0.001 | 11.1 | 1.0 |
| Percutaneous coronary intervention | 1.5 | 2.5 | 0.298 | 0 | 1.0 |
| Coronary artery bypass grafting | 1 | 4.4 | 0.001 | 0 | 1.0 |
| Cardiovascular risk factors (%) | |||||
| Smoking history (%) | |||||
| Never smoked | 35.8 | 34.8 | 0.389 | 33.3 | 0.045 |
| Past smoking | 17.4 | 21.5 | 27.8 | ||
| Current smoking | 46.9 | 43.7 | 38.9 | ||
| Hypertension | 50.1 | 51.3 | 0.773 | 44.4 | 0.631 |
| Diabetes | 14 | 12.7 | 0.637 | 0 | 0.161 |
| Time from symptom onset to randomization (h)a | 3.0 (2.1–4.1) | 3.0 (2.1–4.4) | 0.690 | 3.3 (3.0–3.9) | 0.465 |
| Hemodynamics | |||||
| Systolic blood pressure (mmHg)a | 130 (120–150) | 130 (115–150) | 0.445 | 119.5 (101–130) | 0.004 |
| Heart rate (beats/min)a | 72 (62–84) | 78 (64–90) | 0.002 | 72 (65–80) | 0.848 |
| Killip Class (%) | |||||
| I | 83.4 | 82.3 | 0.335 | 83.3 | 0.323 |
| II | 14.1 | 15.8 | 11.1 | ||
| III | 1.4 | 0 | 0 | ||
| IV | 1.1 | 1.9 | 5.6 | ||
| Randomization to bivalirudin (%) | 49.4 | 49.4 | 0.986 | 33.3 | 0.172 |
| GUSTO risk scorea | 55 (46–66) | 65 (55–74) | <0.001 | 61 (55–76) | 0.030 |
| Peak enzyme level expressed as multiple of ULNa,b | 7.4 (3.7–13.4) | 6.3 (2.8–12.6) | 0.156 | 11.6 (5.3–14.0) | 0.465 |
| In-hospital revascularisation (%) | |||||
| Percutaneous coronary intervention | 6.5 | 6.3 | 0.942 | 5.6 | 1.0 |
| Coronary artery bypass grafting | 0.9 | 0.6 | 1.0 | 0 | 1.0 |
| Mortality (%) | |||||
| Within 30 days | 6.9 | 11.4 | 0.028 | 16.7 | 0.124 |
| Within 24 h | 2.5 | 4.4 | 0.126 | 11.1 | 0.075 |
| . | Inferior AMI with normal conduction at randomization and 60 min (n=8030) . | Inferior AMI with RBBB at randomization (n=158) . | P-value . | Inferior AMI with new RBBB developing within 60 min (n=18) . | P-value . |
|---|---|---|---|---|---|
| Demographics | |||||
| Age (years)a | 60 (51–69) | 68 (60–74) | <0.001 | 65 (59–70) | 0.079 |
| Age ≥75 years (%) | 11.4 | 23.4 | <0.001 | 11.1 | 1.0 |
| Women (%) | 27.8 | 21.5 | 0.080 | 11.1 | 0.114 |
| Previous cardiovascular disease and interventions (%) | |||||
| Angina | 43.3 | 49.4 | 0.128 | 33.3 | 0.394 |
| AMI | 13.4 | 22.8 | 0.001 | 11.1 | 1.0 |
| Percutaneous coronary intervention | 1.5 | 2.5 | 0.298 | 0 | 1.0 |
| Coronary artery bypass grafting | 1 | 4.4 | 0.001 | 0 | 1.0 |
| Cardiovascular risk factors (%) | |||||
| Smoking history (%) | |||||
| Never smoked | 35.8 | 34.8 | 0.389 | 33.3 | 0.045 |
| Past smoking | 17.4 | 21.5 | 27.8 | ||
| Current smoking | 46.9 | 43.7 | 38.9 | ||
| Hypertension | 50.1 | 51.3 | 0.773 | 44.4 | 0.631 |
| Diabetes | 14 | 12.7 | 0.637 | 0 | 0.161 |
| Time from symptom onset to randomization (h)a | 3.0 (2.1–4.1) | 3.0 (2.1–4.4) | 0.690 | 3.3 (3.0–3.9) | 0.465 |
| Hemodynamics | |||||
| Systolic blood pressure (mmHg)a | 130 (120–150) | 130 (115–150) | 0.445 | 119.5 (101–130) | 0.004 |
| Heart rate (beats/min)a | 72 (62–84) | 78 (64–90) | 0.002 | 72 (65–80) | 0.848 |
| Killip Class (%) | |||||
| I | 83.4 | 82.3 | 0.335 | 83.3 | 0.323 |
| II | 14.1 | 15.8 | 11.1 | ||
| III | 1.4 | 0 | 0 | ||
| IV | 1.1 | 1.9 | 5.6 | ||
| Randomization to bivalirudin (%) | 49.4 | 49.4 | 0.986 | 33.3 | 0.172 |
| GUSTO risk scorea | 55 (46–66) | 65 (55–74) | <0.001 | 61 (55–76) | 0.030 |
| Peak enzyme level expressed as multiple of ULNa,b | 7.4 (3.7–13.4) | 6.3 (2.8–12.6) | 0.156 | 11.6 (5.3–14.0) | 0.465 |
| In-hospital revascularisation (%) | |||||
| Percutaneous coronary intervention | 6.5 | 6.3 | 0.942 | 5.6 | 1.0 |
| Coronary artery bypass grafting | 0.9 | 0.6 | 1.0 | 0 | 1.0 |
| Mortality (%) | |||||
| Within 30 days | 6.9 | 11.4 | 0.028 | 16.7 | 0.124 |
| Within 24 h | 2.5 | 4.4 | 0.126 | 11.1 | 0.075 |
aMedian (interquartile range).
bThe peak enzyme level was based on the CK-MB level where available or on the CK level if the CK-MB level was not available.
Table 3 Baseline characteristics and mortality in patients who had inferior AMI with RBBB vs. inferior AMI with normal intraventricular conduction
| . | Inferior AMI with normal conduction at randomization and 60 min (n=8030) . | Inferior AMI with RBBB at randomization (n=158) . | P-value . | Inferior AMI with new RBBB developing within 60 min (n=18) . | P-value . |
|---|---|---|---|---|---|
| Demographics | |||||
| Age (years)a | 60 (51–69) | 68 (60–74) | <0.001 | 65 (59–70) | 0.079 |
| Age ≥75 years (%) | 11.4 | 23.4 | <0.001 | 11.1 | 1.0 |
| Women (%) | 27.8 | 21.5 | 0.080 | 11.1 | 0.114 |
| Previous cardiovascular disease and interventions (%) | |||||
| Angina | 43.3 | 49.4 | 0.128 | 33.3 | 0.394 |
| AMI | 13.4 | 22.8 | 0.001 | 11.1 | 1.0 |
| Percutaneous coronary intervention | 1.5 | 2.5 | 0.298 | 0 | 1.0 |
| Coronary artery bypass grafting | 1 | 4.4 | 0.001 | 0 | 1.0 |
| Cardiovascular risk factors (%) | |||||
| Smoking history (%) | |||||
| Never smoked | 35.8 | 34.8 | 0.389 | 33.3 | 0.045 |
| Past smoking | 17.4 | 21.5 | 27.8 | ||
| Current smoking | 46.9 | 43.7 | 38.9 | ||
| Hypertension | 50.1 | 51.3 | 0.773 | 44.4 | 0.631 |
| Diabetes | 14 | 12.7 | 0.637 | 0 | 0.161 |
| Time from symptom onset to randomization (h)a | 3.0 (2.1–4.1) | 3.0 (2.1–4.4) | 0.690 | 3.3 (3.0–3.9) | 0.465 |
| Hemodynamics | |||||
| Systolic blood pressure (mmHg)a | 130 (120–150) | 130 (115–150) | 0.445 | 119.5 (101–130) | 0.004 |
| Heart rate (beats/min)a | 72 (62–84) | 78 (64–90) | 0.002 | 72 (65–80) | 0.848 |
| Killip Class (%) | |||||
| I | 83.4 | 82.3 | 0.335 | 83.3 | 0.323 |
| II | 14.1 | 15.8 | 11.1 | ||
| III | 1.4 | 0 | 0 | ||
| IV | 1.1 | 1.9 | 5.6 | ||
| Randomization to bivalirudin (%) | 49.4 | 49.4 | 0.986 | 33.3 | 0.172 |
| GUSTO risk scorea | 55 (46–66) | 65 (55–74) | <0.001 | 61 (55–76) | 0.030 |
| Peak enzyme level expressed as multiple of ULNa,b | 7.4 (3.7–13.4) | 6.3 (2.8–12.6) | 0.156 | 11.6 (5.3–14.0) | 0.465 |
| In-hospital revascularisation (%) | |||||
| Percutaneous coronary intervention | 6.5 | 6.3 | 0.942 | 5.6 | 1.0 |
| Coronary artery bypass grafting | 0.9 | 0.6 | 1.0 | 0 | 1.0 |
| Mortality (%) | |||||
| Within 30 days | 6.9 | 11.4 | 0.028 | 16.7 | 0.124 |
| Within 24 h | 2.5 | 4.4 | 0.126 | 11.1 | 0.075 |
| . | Inferior AMI with normal conduction at randomization and 60 min (n=8030) . | Inferior AMI with RBBB at randomization (n=158) . | P-value . | Inferior AMI with new RBBB developing within 60 min (n=18) . | P-value . |
|---|---|---|---|---|---|
| Demographics | |||||
| Age (years)a | 60 (51–69) | 68 (60–74) | <0.001 | 65 (59–70) | 0.079 |
| Age ≥75 years (%) | 11.4 | 23.4 | <0.001 | 11.1 | 1.0 |
| Women (%) | 27.8 | 21.5 | 0.080 | 11.1 | 0.114 |
| Previous cardiovascular disease and interventions (%) | |||||
| Angina | 43.3 | 49.4 | 0.128 | 33.3 | 0.394 |
| AMI | 13.4 | 22.8 | 0.001 | 11.1 | 1.0 |
| Percutaneous coronary intervention | 1.5 | 2.5 | 0.298 | 0 | 1.0 |
| Coronary artery bypass grafting | 1 | 4.4 | 0.001 | 0 | 1.0 |
| Cardiovascular risk factors (%) | |||||
| Smoking history (%) | |||||
| Never smoked | 35.8 | 34.8 | 0.389 | 33.3 | 0.045 |
| Past smoking | 17.4 | 21.5 | 27.8 | ||
| Current smoking | 46.9 | 43.7 | 38.9 | ||
| Hypertension | 50.1 | 51.3 | 0.773 | 44.4 | 0.631 |
| Diabetes | 14 | 12.7 | 0.637 | 0 | 0.161 |
| Time from symptom onset to randomization (h)a | 3.0 (2.1–4.1) | 3.0 (2.1–4.4) | 0.690 | 3.3 (3.0–3.9) | 0.465 |
| Hemodynamics | |||||
| Systolic blood pressure (mmHg)a | 130 (120–150) | 130 (115–150) | 0.445 | 119.5 (101–130) | 0.004 |
| Heart rate (beats/min)a | 72 (62–84) | 78 (64–90) | 0.002 | 72 (65–80) | 0.848 |
| Killip Class (%) | |||||
| I | 83.4 | 82.3 | 0.335 | 83.3 | 0.323 |
| II | 14.1 | 15.8 | 11.1 | ||
| III | 1.4 | 0 | 0 | ||
| IV | 1.1 | 1.9 | 5.6 | ||
| Randomization to bivalirudin (%) | 49.4 | 49.4 | 0.986 | 33.3 | 0.172 |
| GUSTO risk scorea | 55 (46–66) | 65 (55–74) | <0.001 | 61 (55–76) | 0.030 |
| Peak enzyme level expressed as multiple of ULNa,b | 7.4 (3.7–13.4) | 6.3 (2.8–12.6) | 0.156 | 11.6 (5.3–14.0) | 0.465 |
| In-hospital revascularisation (%) | |||||
| Percutaneous coronary intervention | 6.5 | 6.3 | 0.942 | 5.6 | 1.0 |
| Coronary artery bypass grafting | 0.9 | 0.6 | 1.0 | 0 | 1.0 |
| Mortality (%) | |||||
| Within 30 days | 6.9 | 11.4 | 0.028 | 16.7 | 0.124 |
| Within 24 h | 2.5 | 4.4 | 0.126 | 11.1 | 0.075 |
aMedian (interquartile range).
bThe peak enzyme level was based on the CK-MB level where available or on the CK level if the CK-MB level was not available.
Table 4 Thirtyday mortality in patients with the different types of BBB at randomization or developing newly within 60 min after commencement of fibrinolytic therapy
| . | Unadjusted OR (95% CI)a . | OR (95% CI) adjusted for recruitment region and pre-infarction characteristicsb . | OR (95% CI) adjusted for recruitment region, pre-infarction characteristicsb and presenting featuresc . |
|---|---|---|---|
| LBBBd | |||
| Left BBB at randomization | 1.90 (1.39–2.59) | 1.10 (0.79–1.53) | 0.69 (0.48–0.99) |
| New LBBB developing within 60 min | 4.68 (2.02–10.87) | 3.17 (1.27–7.89) | 2.97 (1.16–7.57) |
| Anterior AMI with RBBBe | |||
| RBBB at randomization | 3.52 (2.82–4.38) | 3.24 (2.55–4.11) | 2.48 (1.93–3.19) |
| New RBBB developing within 60 min | 3.75 (2.46–5.73) | 4.15 (2.61–6.61) | 3.84 (2.38–6.22) |
| Inferior AMI with RBBBf | |||
| RBBB at randomization | 1.74 (1.06–2.86) | 1.21 (0.72–2.03) | 1.22 (0.71–2.08) |
| New RBBB developing within 60 min | 2.71 (0.78–9.38) | 3.08 (0.85–11.22) | 2.23 (0.54–9.21) |
| . | Unadjusted OR (95% CI)a . | OR (95% CI) adjusted for recruitment region and pre-infarction characteristicsb . | OR (95% CI) adjusted for recruitment region, pre-infarction characteristicsb and presenting featuresc . |
|---|---|---|---|
| LBBBd | |||
| Left BBB at randomization | 1.90 (1.39–2.59) | 1.10 (0.79–1.53) | 0.69 (0.48–0.99) |
| New LBBB developing within 60 min | 4.68 (2.02–10.87) | 3.17 (1.27–7.89) | 2.97 (1.16–7.57) |
| Anterior AMI with RBBBe | |||
| RBBB at randomization | 3.52 (2.82–4.38) | 3.24 (2.55–4.11) | 2.48 (1.93–3.19) |
| New RBBB developing within 60 min | 3.75 (2.46–5.73) | 4.15 (2.61–6.61) | 3.84 (2.38–6.22) |
| Inferior AMI with RBBBf | |||
| RBBB at randomization | 1.74 (1.06–2.86) | 1.21 (0.72–2.03) | 1.22 (0.71–2.08) |
| New RBBB developing within 60 min | 2.71 (0.78–9.38) | 3.08 (0.85–11.22) | 2.23 (0.54–9.21) |
aAdjustment for the recruitment region resulted in minimal changes of the ORs for mortality.
bPreinfarction characteristics included age, gender, previous AMI, previous coronary or vascular disease, diabetes mellitus, and smoking. Further adjustment for the time to randomization resulted in minimal changes of the ORs for mortality.
cPresenting features included the time to randomization, systolic blood pressure, pulse rate, and Killip class.
dVs. patients who had any AMI with normal intraventricular conduction.
eVs. patients who had anterior AMI with normal intraventricular conduction.
fVs. patients who had inferior AMI with normal intraventricular conduction.
Table 4 Thirtyday mortality in patients with the different types of BBB at randomization or developing newly within 60 min after commencement of fibrinolytic therapy
| . | Unadjusted OR (95% CI)a . | OR (95% CI) adjusted for recruitment region and pre-infarction characteristicsb . | OR (95% CI) adjusted for recruitment region, pre-infarction characteristicsb and presenting featuresc . |
|---|---|---|---|
| LBBBd | |||
| Left BBB at randomization | 1.90 (1.39–2.59) | 1.10 (0.79–1.53) | 0.69 (0.48–0.99) |
| New LBBB developing within 60 min | 4.68 (2.02–10.87) | 3.17 (1.27–7.89) | 2.97 (1.16–7.57) |
| Anterior AMI with RBBBe | |||
| RBBB at randomization | 3.52 (2.82–4.38) | 3.24 (2.55–4.11) | 2.48 (1.93–3.19) |
| New RBBB developing within 60 min | 3.75 (2.46–5.73) | 4.15 (2.61–6.61) | 3.84 (2.38–6.22) |
| Inferior AMI with RBBBf | |||
| RBBB at randomization | 1.74 (1.06–2.86) | 1.21 (0.72–2.03) | 1.22 (0.71–2.08) |
| New RBBB developing within 60 min | 2.71 (0.78–9.38) | 3.08 (0.85–11.22) | 2.23 (0.54–9.21) |
| . | Unadjusted OR (95% CI)a . | OR (95% CI) adjusted for recruitment region and pre-infarction characteristicsb . | OR (95% CI) adjusted for recruitment region, pre-infarction characteristicsb and presenting featuresc . |
|---|---|---|---|
| LBBBd | |||
| Left BBB at randomization | 1.90 (1.39–2.59) | 1.10 (0.79–1.53) | 0.69 (0.48–0.99) |
| New LBBB developing within 60 min | 4.68 (2.02–10.87) | 3.17 (1.27–7.89) | 2.97 (1.16–7.57) |
| Anterior AMI with RBBBe | |||
| RBBB at randomization | 3.52 (2.82–4.38) | 3.24 (2.55–4.11) | 2.48 (1.93–3.19) |
| New RBBB developing within 60 min | 3.75 (2.46–5.73) | 4.15 (2.61–6.61) | 3.84 (2.38–6.22) |
| Inferior AMI with RBBBf | |||
| RBBB at randomization | 1.74 (1.06–2.86) | 1.21 (0.72–2.03) | 1.22 (0.71–2.08) |
| New RBBB developing within 60 min | 2.71 (0.78–9.38) | 3.08 (0.85–11.22) | 2.23 (0.54–9.21) |
aAdjustment for the recruitment region resulted in minimal changes of the ORs for mortality.
bPreinfarction characteristics included age, gender, previous AMI, previous coronary or vascular disease, diabetes mellitus, and smoking. Further adjustment for the time to randomization resulted in minimal changes of the ORs for mortality.
cPresenting features included the time to randomization, systolic blood pressure, pulse rate, and Killip class.
dVs. patients who had any AMI with normal intraventricular conduction.
eVs. patients who had anterior AMI with normal intraventricular conduction.
fVs. patients who had inferior AMI with normal intraventricular conduction.
References
Fibrinolytic Therapy Trialists’ (FTT) Collaborative Group. Indications for fibrinolytic therapy in suspected acute myocardial infarction: collaborative overview of early mortality and major morbidity results from all randomised trials of more than 1000 patients.
Newby KH, Pisano E, Krucoff MW, Green C, Natale A. Incidence and clinical relevance of the occurrence of bundle-branch block in patients treated with thrombolytic therapy.
Morrow DA, Antman EM, Charlesworth A, Cairns R, Murphy SA, de Lemos JA, Giugliano RP, McCabe CH, Braunwald E. TIMI risk score for ST-elevation myocardial infarction: a convenient, bedside, clinical score for risk assessment at presentation: an Intravenous nPA for Treatment of Infarcting Myocardium Early II trial substudy.
Califf RM, Woodlief LH, Harrell FE Jr, Lee KL, White HD, Guerci A, Barbash GI, Simes RJ, Weaver WDD, Simoons ML, Topol EJ for the GUSTO-I Investigators. Selection of thrombolytic therapy for individual patients: development of a clinical model.
The Hirulog and Early Reperfusion or Occlusion (HERO)-2 Trial Investigators. Thrombin-specific anticoagulation with bivalirudin versus heparin in patients receiving fibrinolytic therapy for acute myocardial infarction: the HERO-2 randomised trial.
Sgarbossa EB, Pinski SL, Barbagelata A, Underwood DA, Gates KB, Topol EJ, Califf RM, Wagner GS for the GUSTO-1 (Global Utilization of Streptokinase and Tissue Plasminogen Activator for Occluded Coronary Arteries) Investigators. Electrocardiographic diagnosis of evolving acute myocardial infarction in the presence of left bundle-branch block.
Willems JL, Robles de Medina EO, Bernard R, Coumel P, Fisch C, Krikler D, Mazur NA, Meijler FL, Mogensen L, Moret P, Pisa Z, Rautaharju PM, Surawicz B, Watanabe Y, Wellens HJJ. Criteria for intraventricular conduction disturbances and pre-excitation. World Health Organizational/International Society and Federation for Cardiology Task Force Ad Hoc.
Kleiman NS, White HD, Ohman EM, Ross AM, Woodlief LH, Califf RM, Holmes DR Jr, Bates E, Pfisterer M, Vahanian A, Topol EJ for the GUSTO Investigators. Mortality within 24 hours of thrombolysis for myocardial infarction: the importance of early reperfusion.
Rubart M, Zipes DP. Genesis of cardiac arrhythmias: electrophysiological considerations. In: Zipes DP, Libby P, Bonow RO, Braunwald E eds.
Antman EM, Anbe DT, Armstrong PW, Bates ER, Green LA, Hand M, Hochman JS, Krumholz HM, Kushner FG, Lamas GA, Mullany CJ, Ornato JP, Pearle DL, Sloan MA, Smith SC Jr. ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction—executive summary. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to revise the 1999 guidelines for the management of patients with acute myocardial infarction).
Van de Werf F, Ardissino D, Betriu A, Cokkinos DV, Falk E, Fox KAA, Julian D, Lengyel M, Neumann FJ, Ruzyllo W, Thygesen C, Underwood SR, Vahanian A, Verheugt FWA, Wijns W. Management of acute myocardial infarction in patients presenting with ST-segment elevation: the Task Force on the Management of Acute Myocardial Infarction of the European Society of Cardiology.
Wong CK, French JK, Aylward PE, Stewart RA, Gao W, Armstrong PW, Van de Werf FJ, Simes RJ, Raffel OC, Granger CB, Califf RM, White HD. Patients with prolonged ischemic chest pain and presumed-new left bundle branch block have heterogeneous outcomes depending on the presence of ST-segment changes.
Sgarbossa EB, Pinski SL, Topol EJ, Califf RM, Barbagelata A, Goodman SG, Gates KB, Granger CB, Miller DP, Underwood DA, Wagner GS for the GUSTO-1 Investigators. Acute myocardial infarction and complete bundle branch block at hospital admission: clinical characteristics and outcome in the thrombolytic era.
Kontos MC, McQueen RH, Jesse RL, Tatum JL, Ornato JP. Can myocardial infarction be rapidly identified in emergency department patients who have left bundle-branch block?
Gula LJ, Dick A, Massel D. Diagnosing acute myocardial infarction in the setting of left bundle branch block: prevalence and observer variability from a large community study.
Melgarejo-Moreno A, Galcera-Tomas J, Garcia-Alberola A, Valdes-Chavarri M, Castillo-Soria FJ, Mira-Sanchez E, Gil-Sanchez J, Allegue-Gallego J. Incidence, clinical characteristics, and prognostic significance of right bundle-branch block in acute myocardial infarction: a study in the thrombolytic era.
Scheinman M, Brenman B. Clinical and anatomic implications of intraventricular conduction blocks in acute myocardial infarction.
Norris RM, Croxson MS. Bundle branch block in acute myocardial infarction.
Scheidt S, Killip T. Bundle-branch block complicating acute myocardial infarction.
Hindman MC, Wagner GS, JaRo M, Atkins JM, Scheinman MM, DeSanctis RW, Hutter AH Jr, Yeatman L, Rubenfire M, Pujura C, Rubin M, Morris JJ. The clinical significance of bundle branch block complicating acute myocardial infarction. 1. Clinical characteristics, hospital mortality, and one-year follow-up.
Dubois C, Pierard LA, Smeets JP, Foidart G, Legrand V, Kulbertus HE. Short- and long-term prognostic importance of complete bundle-branch block complicating acute myocardial infarction.
Fernandez-Aviles F, Alonso JJ, Castro-Beiras A, Vazquez N, Blanco J, Alonso-Briales J, Lopez-Mesa J, Fernandez-Vazquez F, Calvo I, Martinez-Elbal L, San Roman JA, Ramos B. Routine invasive strategy within 24 hours of thrombolysis versus ischaemia-guided conservative approach for acute myocardial infarction with ST-segment elevation (GRACIA-1): a randomised controlled trial.
Van de Werf F, Gore JM, Avezum A, Gulba DC, Goodman SG, Budaj A, Brieger D, White K, Fox KA, Eagle KA, Kennelly BM. Access to catheterisation facilities in patients admitted with acute coronary syndrome: multinational registry study.
Sutton AG, Campbell PG, Graham R, Price DJ, Gray JC, Grech ED, Hall JA, Harcombe AA, Wright RA, Smith RH, Murphy JJ, Shyam-Sundar A, Stewart MJ, Davies A, Linker NJ, de Belder MA. A randomized trial of rescue angioplasty versus a conservative approach for failed fibrinolysis in ST-segment elevation myocardial infarction: the Middlesbrough Early Revascularization to Limit INfarction (MERLIN) trial.
Hochman JS, Sleeper LA, Webb JG, Sanborn TA, White HD, Talley JD, Buller CE, Jacobs AK, Slater JN, Col J, McKinlay SM, LeJemtel TH, Picard MH, Menegus MA, Boland J, Dzavik V, Thompson CR, Wong SC, Steingart R, Forman R, Aylward PE, Godfrey E, Desvigne-Nickens P for the SHOCK Investigators. Early revascularization in acute myocardial infarction complicated by cardiogenic shock.