Abstract
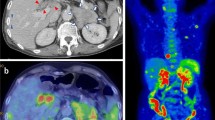
A 64-year-old man with a history of chronic lymphocytic leukemia (CLL) presented in the hematology department due to remarkable leukocytosis and progressing anemia. Ultrasound confirmed splenomegaly and plain computed tomography revealed multiple hypoattenuating areas in the large spleen. Following a clinical diagnosis of relapse of CLL, he underwent treatment with fludarabine, cyclophosphamide, and rituximab (FC-R). After five cycles of FC-R treatment, his leukocyte count and hemoglobin level were normalized, and the size of the spleen also decreased. He began to have intermittent high fever (38 °C), however, approximately 6 months after the initiation of FC-R treatment. The results of an interferon-gamma release assay were positive. 18F-fluoro-2-deoxy-d-glucose positron emission tomography showed multiple areas of high-uptake in the spleen, which was unclear in other radiologic modalities. We performed a splenectomy for the high fever and to confirm the diagnosis. Tissue cultures of the infarcted area of spleen were positive for Propionibacterium acnes. After splenectomy, the patient’s condition improved and there were no further episodes of fever. Until recently, three cases of splenic abscess caused by Propionibacterium acnes were reported. Here we present a fourth case of splenic abscess due to Propionibacterium acnes and review the literature.


Similar content being viewed by others
References
Levy PY, et al. Propionibacterium acnes postoperative shoulder arthritis: an emerging clinical entity. Clin Infect Dis. 2008;46(12):1884–6.
Perry A, Lambert P. Propionibacterium acnes: infection beyond the skin. Expert Rev Anti Infect Ther. 2011;9(12):1149–56.
Harris AE, et al. Postoperative discitis due to Propionibacterium acnes: a case report and review of the literature. Surg Neurol. 2005;63(6):538–41 (discussion 541).
Gekowski KM, et al. Splenic abscess caused by Propionibacterium acnes. Yale J Biol Med. 1982;55(1):65–9.
Gangahar DM, Delany HM. Intrasplenic abscess: two case reports and review of the literature. Am Surg. 1981;47(11):488–91.
Chang KC, et al. Clinical characteristics and prognostic factors of splenic abscess: a review of 67 cases in a single medical center of Taiwan. World J Gastroenterol. 2006;12(3):460–4.
Nelken N, et al. Changing clinical spectrum of splenic abscess. A multicenter study and review of the literature. Am J Surg. 1987;154(1):27–34.
Chun CH, et al. Splenic abscess. Medicine (Baltimore). 1980;59(1):50–65.
Antopolsky M, et al. Splenic infarction: 10 years of experience. Am J Emerg Med. 2009;27(3):262–5.
Lee WS, Choi ST, Kim KK. Splenic abscess: a single institution study and review of the literature. Yonsei Med J. 2011;52(2):288–92.
Vanderschueren S, et al. From prolonged febrile illness to fever of unknown origin: the challenge continues. Arch Intern Med. 2003;163(9):1033–41.
Kubota K, et al. FDG-PET for the diagnosis of fever of unknown origin: a Japanese multi-center study. Ann Nucl Med. 2011;25(5):355–64.
Niazi SA, et al. Propionibacterium acnes and Staphylococcus epidermidis isolated from refractory endodontic lesions are opportunistic pathogens. J Clin Microbiol. 2010;48(11):3859–69.
Ishige I, et al. Quantitative PCR of mycobacterial and propionibacterial DNA in lymph nodes of Japanese patients with sarcoidosis. Lancet. 1999;354(9173):120–3.
Jakab E, et al. Severe infections caused by Propionibacterium acnes: an underestimated pathogen in late postoperative infections. Yale J Biol Med. 1996;69(6):477–82.
O’Brien SM, et al. Results of the fludarabine and cyclophosphamide combination regimen in chronic lymphocytic leukemia. J Clin Oncol. 2001;19(5):1414–20.
Ooi LL, Leong SS. Splenic abscesses from 1987 to 1995. Am J Surg. 1997;174(1):87–93.
Ferraioli G, et al. Management of splenic abscess: report on 16 cases from a single center. Int J Infect Dis. 2009;13(4):524–30.
Llenas-Garcia J, et al. Splenic abscess: a review of 22 cases in a single institution. Eur J Intern Med. 2009;20(5):537–9.
Park HJ, et al. Clinical significance of Propionibacterium acnes recovered from blood cultures: analysis of 524 episodes. J Clin Microbiol. 2011;49(4):1598–601.
Eishi Y, et al. Quantitative analysis of mycobacterial and propionibacterial DNA in lymph nodes of Japanese and European patients with sarcoidosis. J Clin Microbiol. 2002;40(1):198–204.
Roberts SA, et al. Antimicrobial susceptibility of anaerobic bacteria in New Zealand: 1999–2003. J Antimicrob Chemother. 2006;57(5):992–8.
Kawada A, Aragane Y, Tezuka T. Levofloxacin is effective for inflammatory acne and achieves high levels in the lesions: an open study. Dermatology. 2002;204(4):301–2.
Acknowledgments
The authors would like to thank Masako Sugimoto, Yasuhiko Kamikubo, Mineo Kurokawa of Department of Hematology, Graduate School of Medicine, The University of Tokyo, Yukako Shintani, Masashi Fukayama of Department of Pathology, Graduate School of Medicine, The University of Tokyo, Junichi Shindoh, Yoshikuni Kawaguchi, Kiyohiko Omichi, Hepato-Biliary-Pancreatic Surgery, Artificial Organ and Transplantation Division, Department of Surgery, Graduate School of Medicine, The University of Tokyo for their important contributions to the diagnosis.
Disclosures
Conflict of Interest: The authors declare that they have no conflict of interest.
Human/Animal Rights: All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008(5).
Informed Consent: Informed consent was obtained from all patients for being included in the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kiritani, S., Kaneko, J., Aoki, T. et al. Multiple splenic nodules with fever: a case of splenic abscess due to Propionibacterium acnes . Clin J Gastroenterol 6, 434–437 (2013). https://doi.org/10.1007/s12328-013-0427-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12328-013-0427-5