Abstract
Introduction
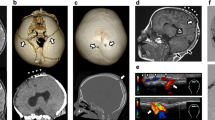
Sinus pericranii (SP) is a rare, usually asymptomatic condition characterized by a large communication between the intra- and the extracranial venous drainage pathways in which blood may circulate bidirectionally through dilated veins of the skull. We describe our diagnostic and therapeutic experience with SP, with a special focus on the vascular analysis of digital subtraction angiography (DSA).
Methods
DSA images of 15 patients were evaluated with regard to the delay in opacification of the scalp vessels, the absence or distortion of the superficial cortical veins in the vicinity of the SP, the drainage patterns of the superior sagittal sinus, and the degree of maturation of the venous outlets of the brain. SP were classified either as “dominant”, if the main stream of contrast flow used the SP to drain the brain bypassing usual venous outlets, or as “accessory”, if only a small part of the venous outflow occurred through the extradiploic vessels.
Results
All patients presented with a nonpulsatile, soft-tissue mass. The lesion was on the midline in 14 of 15 patients, frontal in 12 patients, and parietal in 2 patients. In 13 patients, associated intracranial venous anomalies were present, eight of which were developmental venous anomalies. Seven patients had a dominant SP, and eight an accessory SP.
Conclusion
SP can be considered the cutaneous sign of an underlying venous anomaly. If treatment is contemplated, analysis of the drainage pattern of the SP has to be performed. Treatment should be avoided in dominant SP or if its accessory role constitutes the only collateral pathway of an underlying venous anomaly.




Similar content being viewed by others
References
Stromeyer (1993) About sinus pericranii (translating of original 1850 text). Surg Neurol 40:3–4
Anegawa S, Hayashi T, Torigoe R, Nakagawa S, Ogasawara T (1991) Sinus pericranii with severe symptom due to transient disorder of venous return – case report. Neurol Med Chir (Tokyo) 31:287–289
Carpenter JS, Rosen CL, Bailes JE, Gailloud P (2004) Sinus pericranii: clinical and imaging findings in two cases of spontaneous partial thrombosis. AJNR Am J Neuroradiol 25:121–125
Marras C, McEvoy AW, Grieve JP, Jager HR, Kitchen ND, Villani RM (2001) Giant temporo-occipital sinus pericranii. A case report. J Neurosurg Sci 45:103–109
Ota T, Waga S, Handa H, Nishimura S, Mitani T (1975) Sinus pericranii. J Neurosurg 42:704–712
Sheu M, Fauteux G, Chang H, Taylor W, Stopa E, Robinson-Bostom L (2002) Sinus pericranii: dermatologic considerations and literature review. J Am Acad Dermatol 46:934–941
Vinas FC, Valenzuela S, Zuleta A (1994) Literature review: Sinus pericranii. Neurol Res 16:471–474
Wakisaka S, Okuda S, Soejima T, Tsukamoto Y (1983) Sinus pericranii. Surg Neurol 19:291–298
Bigot JL, Iacona C, Lepreux A, Dhellemmes P, Motte J, Gomes H (2000) Sinus pericranii: advantages of MR imaging. Pediatr Radiol 30:710–712
Bollar A, Allut AG, Prieto A, Gelabert M, Becerra E (1992) Sinus pericranii: radiological and etiopathological considerations. J Neurosurg 77:469–472
Witrak BJ, Davis PC, Hoffmann JCJ (1986) Sinus pericranii. A case report. Pediatr Radiol 16:55–56
Wen CS, Chang YL, Wang HS, Kuo MF, Tu YK (2005) Sinus pericranii: from gross and neuroimaging findings to different pathophysiological changes. Childs Nerv Syst 21:482–488
Lasjaunias P (1997) Vascular diseases in neonates, infants and children: interventional neuroradiology management. Springer, Berlin Heidelberg New York
Tortori-Donati P, Rossi A (2005) Pediatric neuroradiology. Springer, Berlin Heidelberg New York
David LR, Argenta LC, Venes J, Wilson J, Galzier S (1998) Sinus pericranii. J Craniofac Surg 9:3–10
Spektor S, Weinberger G, Constantini S, Gomori JM, Beni-Adani L (1998) Giant lateral sinus pericranii: case report. J Neurosurg 88:145–147
Nozaki J, Kawano H, Kabuto M, Hirose K, Hayashi M (1986) Lateral sinus pericranii. Surg Neurol 25:487–490
Sakai K, Namba K, Meguro T et al (1997) Sinus pericranii associated with a cerebellar venous angioma: case report. Neurol Med Chir (Tokyo) 37:464–467
Nomura S, Kato S, Ishihara H, Yoneda H, Ideguchi M, Suzuki M (2006) Association of intra- and extradural venous anomalies, so-called venous angioma and sinus pericranii. Childs Nerv Syst 22:428–431
Nakasu Y, Nakasu S, Minouchi K, Handa J (1993) Multiple sinus pericranii with systemic angiomas: case report. Surg Neurol 39:41–45
Beers GJ, Carter AP, Ordia JI, Shapiro M (1984) Sinus pericranii with dural venous lakes. AJNR Am J Neuroradiol 5:626–631
Nakayama T, Matsukado Y (1975) Sinus pericranii with aneurysmal malformation of the internal cerebral vein. Surg Neurol 3:133–137
Sherry RG, Walker ML, Olds MV (1984) Sinus pericranii and venous angioma in the blue-rubber bleb nevus syndrome. AJNR Am J Neuroradiol 5:832–834
Lasjaunias P, Kwok R, Goh P, Yeong KY, Lim W, Chng SM (2004) A developmental theory of the superior sagittal sinus(es) in craniopagus twins. Childs Nerv Syst 20:526–537
Nishio A, Sakaguchi M, Murata K, Nishikawa M, Nishimura S (1989) Lateral situated sinus pericranii. Case report. Surg Neurol 32:382–386
Brisman JL, Niimi Y, Berenstein A (2004) Sinus pericranii Involving the torcular sinus in a patient with Hunter’s syndrome and trigonocephaly: case report and review of the literature. Neurosurgery 55:433
Kurosu A, Wachi A, Bando K, Kumami K, Naito S, Sato K (1994) Craniosynostosis in the presence of a sinus pericranii: case report. Neurosurgery 34:1090–1092
Yasuda S, Enomoto T, Yamada Y, Nose T, Iwasaki N (1993) Crouzon disease associated with sinus pericranii: a report on identical twin sisters. Childs Nerv Syst 9:119–122
Higuchi M, Fujimoto Y, Ikeda H, Kato A (1997) Sinus pericranii: neuroradiologic findings and clinical management. Pediatr Neurosurg 27:325–328
Acknowledgements
We would like to thank Prof. Guy Wilms and one anonymous reviewer for their careful reading of the manuscript, their thoughtful comments, and their very helpful suggestions concerning the different definitions of SP.
Conflict of interest statement
We declare that we have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Carlo Gandolfo and Timo Krings contributed equally to this work.
Appendix: Clinical and imaging questionnaire
Appendix: Clinical and imaging questionnaire
-
A.
General assessment
List of questions for clinical assessment; if an answer is “No” skip to Pretreatment assessment.
-
AI.
Clinical assessment
-
Has any other differential diagnosis been excluded (haemangioma, cephalocele, venous malformation, etc)?
-
Is the SP located in a typical midline position?
-
Are cosmetic problems the only complaint? If no, specify (physical, e.g. size, position or associated dermatological problems; clinical, e.g. visual impairment, headache, bleeding, pain)
-
Can the clinical or physical complaints be treated conservatively?
-
Is there any premature syndromic or non-syndromic fusion of the cranial sutures (craniosynostosis, achondroplasia, etc)?
-
-
AII.
Psychological assessment
-
If the cosmetic problem is the main complaint, is the problem tolerable?
-
Can the patient or the patient’s parents understand that treating a venous anomaly is not mandatory and could be associated with a life-threatening risk? Do they agree with the decision to abstain from treatment?
-
Is the psychological, social and academic development of the patient normal?
-
-
AI.
-
B.
Pretreatment assessment
If treatment (surgical or endovascular) is under consideration, CT (bone window), MRI (angiographic study, MRA) and DSA (studying the late venous phase) must be performed or reviewed; ‘negative’ answers point to abstention from treatment.
-
BI.
CT
-
Is the bony communication between the intra- and extracranial compartments subjacent to the SP single and well-marginated?
-
Have phleboliths been searched for and then excluded (within the lesion)?
-
-
BII.
MRI (MRA and phase-contrast sequence for flow-MRI)
-
Is there a no-flow or slow-flow connection between the SP and the intracranial sinus system?
-
Have any associated venous malformations near the SP been excluded?
-
-
BIII.
DSA
-
Is the role of the SP in the global venous drainage accessory (see main text)?
-
If an associated subjacent venous malformation is present, is the role of the SP in the local venous drainage accessory?
-
Are the normal cerebral venous outlets patent?
-
Are the jugular bulbs mature?
-
-
C.
Treatment
The choice of treatment depends on the physical and clinical features of the SP as well as on the experience of the treating team and the wishes of the patient. Endovascular embolization can be presurgical
-
CI.
Surgical. In patients with an uncomplicated, small, thin-linked, soft SP
-
CII.
Endovascular. In patients with a wide-linked, large, stretched-out SP
-
Transvenous (gluing and/or coiling)
-
Percutaneous (gluing)
-
-
CIII.
Abstention from treatment
-
CI.
-
BI.
Rights and permissions
About this article
Cite this article
Gandolfo, C., Krings, T., Alvarez, H. et al. Sinus pericranii: diagnostic and therapeutic considerations in 15 patients. Neuroradiology 49, 505–514 (2007). https://doi.org/10.1007/s00234-007-0211-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-007-0211-7