Abstract
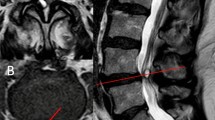
Spinal synovial cysts are cystic dilatations of the synovial membrane that may arise at all levels of the spine. We describe our experience, paying attention to diagnosis, surgical treatment, and long-term follow-up. Between 1995 and 2007, 18 patients were surgically treated. Of these, three patients were excluded from the study because they presented spinal instability at pre-operative assessment. All patients were evaluated pre-operatively with CT, MRI, and dynamic X-rays, and underwent surgery for removal of the cyst by hemilaminectomy and partial arthrectomy. All patients were evaluated with early MRI and had a minimum 2-year follow-up by dynamic X-rays. None of the patients required instrumented fusion due to the absence of radiological signs of instability on the pre-operative dynamic tests. In all patients, there was an immediate resolution of the symptoms, with evidence of complete removal of the cysts on post-operative MRI. At 2-year follow-up, all patients underwent dynamic X-rays and responded to a questionnaire for evaluation of outcome. None of them showed signs of relapse. The gold standard for treatment is surgery, even though other conservative treatment regimens have been proposed. Correct surgical strategy relies on pre-operative assessment of biomechanical stability for deciding whether patients need instrumented fusion during cyst removal. Patients with no instability signs are suitable for hemilaminectomy with partial arthrectomy, preserving 2/3 of the medial portion of the articular facet, because this represents a valid option of treatment with a low risk of complications and a low rate of relapse.





Similar content being viewed by others
References
Christophis P, Asamoto S, Kuchelmeister K, Schachenmayr W (2007) ”Juxtafacet cysts”, a misleading name for cystic formations of mobile spine (CYFMOS). Eur Spine J 16:1499–1505
Amir M, Girardi KF (2006) Spinal lumbar synovial cysts. Diagnosis and management challenge. Eur Spine J 15:1176–1182
Ayberk G et al (2008) Lumbar synovial cyst: experience with nine cases. Neurol Med Chir (Tokyo) 48:298–303
Finkelstein SD, Sayegh R, Watson P, Knuckey N (1993) Juxta-facet cysts. Report of two cases and review of the clinicopathological features. Spine 18:779782
Vernet O, Frankhauser H, Schnyder P, Déruaz JP (1991) Cyst of the ligamentum flavum: report of six cases. Neurosurgery 29:277–283
Ramieri A, Domenicucci TM, Seferi A, Paolini S, Petrozza V, Delfini R (2006) Lumbar hemorrhagic synovial cysts: diagnosis, pathogenesis, and treatment. Report of 3 cases. Surgical Neurology 65:385–390
Onofrio BM, Mih AD (1988) Synovial cysts of the spine. Neurosurgery 22:642–647
Sachdev VP, Savitz MH, Hindi AI, Goldstein HB (1991) Synovial cysts of the lumbar facet joint. Mt Sinai J Med 58:125–128
Boviatsis EJ, Staurinou LC, Kouyialis AT, Gavra MM, Stavrinou PC, Themistokleous M, Selviaridis P, Sakas DE (2008) Spinal synovial cysts: pathogenesis, diagnosis and surgical treatment in a series of seven cases and literature review. Eur Spine J 17:831–837
Shah RV, Lutz GE (2003) Lumbar intraspinal synovial cysts: conservative management and review of the world's literature. Spine J 3:479–488
Yarde WL, Arnold PM, Kepes JJ, O'Boynick PL, Wilkinson SB, Batnitzky S (1995) Spine: synovial cysts of the lumbar spine: diagnosis, surgical management, and pathogenesis report of eight cases. Surg Neurol 43:459–465
Lyons MK, Atkinson JLD, Wharen RE, Deen HG, Zimmerman RS, Lemens SM (2000) Surgical evaluation and management of lumbar synovial cyst. The Mayo Clinic experience. J Neurosurg Spine 93:53–57
Jackson DE, Atlas SW, Mani JR, Norman D (1989) Intraspinal synovial cysts: magnetic resonance imaging. Radiology 170:527–530
Khalatbari K, Ansari H (2008) MRI of degenerative cysts of the lumbar spine. Clin Radiol 63:322e–328e
Wang AM, Haykal HA, Lin JC, Lee JH (1987) Synovial cysts of the lumbar spine: CT evaluation. Compu Radiol 11:253–257
Epstein NE (2004) Lumbar laminectomy for the resection of synovial cysts and coexisting lumbar spinal stenosis or degenerative spondylolisthesis: an outcome study. Spine 29(9):1049–1056
Terao T, Takahashi H, Tanigughi M, Ide K, Shinozaki M, Nakauchi I, Kubota M (2007) Clinical characteristics and surgical managment for juxtafacet cysts of the lumbar spine. Neurol Med Chir (Tokyo) 47:250–257
Imai K, Nakamura K, Inokuchi K, Oda H (1998) Aspiration of intraspinal synovial cyst: recurrence after temporal improvement. Arch Orthop Trauma Surg 118(1–2):103–105
Parlier-Cuau C, Wybier M, Nizard R et al (1999) Symptomatic lumbar facet joint synovial cysts: clinical assessment of facet joint steroid injection after 1 and 6 months and long-term follow-up in 30 patients. Radiology 210:509–513
Banning CS, Thorell WE, Leibrock LG (2001) Patient outcome after resection of lumbar juxtafacet cysts. Spine 26(8):969–972
Sandhu FS, Santiago P, Fessler RG, Palmer S (2004) Minimally invasive surgical treatment of lumbar synovial cysts. Neurosurgery 54(1):107–111
Freidberg SR, Fellows T, Thomas CB et al (1994) Experience with symptomatic spinal epidural cysts. Neurosurgery 34:989–993
Nouzhan S, Khoo LT, Holly LT (2006) Treatment of lumbar synovial cysts using minimally invasive surgical techniques. Neurosurg Focus 20(3):E2
Gökmen Kah‹Lo⁄Ullari Hakan Tuna Ayhan Attar (2008) Management of spinal synovial cysts spinal sinovial kistler. Turkish Neurosurgery 18(2): 211–214
Bydon A, Xu R, Parker SL, McGirt MJ, Bydon M, Gokaslan ZL, Witham TF (2010) Recurrent back and leg pain and cyst reformation after surgical resection of spinal synovial cysts: systematic review of reported postoperative outcomes. Spine J 10:820–826
Author information
Authors and Affiliations
Corresponding author
Additional information
Comments
Imad N. Kanaan, Riyadh, Kingdom of Saudi Arabia
The manuscript represents a retrospective analysis of 15 cases of unilateral lumbar synovial cysts treated with microsurgical excisions and subjected to 2-year follow-ups and outcome study. Synovial cystic dilatation juxtaposing the spinal facet joint is caused by overproduction of synovial fluid and thinning of the overlying facet joint capsule. It occurs mostly in older age in association with advanced degenerative osteoarthritis. The osseous confines of the lateral recess often magnify the degree of impingement on neural structures, and hemorrhage may lead to urgent condition as reported by the authors.
Spinal synovial cyst is relatively rare as correctly stated by the authors but becoming a well-documented cause of compressive radiculopathy and lumbar spine stenosis, thanks to the use of modern imaging facilities of MRI and CTs. The absence of randomization and lack of control was apparently due to a small cohort and rarity of symptomatic disease, but also partially induced by selection bias and single-out treatment option. The evidence is based on case-series reviews coupled with a hint of authoritative statement, but on the other hand, is compensated by an objective review of the literature. The authors should be commended on their meticulous follow-up documentation and outcome results. We concur with the authors that the mainstay in this microsurgical intervention is to limit the arthrectomy and maintain the integrity of 2/3 of the medial facet joint to avoid instability. As a final note, physicians involved in the management of such disease entities should be aware of recent molecular biology research and development and the role of proteinases, collagenases, cadherin-1, and lubrican as potential substrates for future medical treatment option.
Rights and permissions
About this article
Cite this article
Landi, A., Marotta, N., Tarantino, R. et al. Microsurgical excision without fusion as a safe option for resection of synovial cyst of the lumbar spine: long-term follow-up in mono-institutional experience. Neurosurg Rev 35, 245–253 (2012). https://doi.org/10.1007/s10143-011-0356-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-011-0356-z